Pharyngectomy
You have been referred this page because you, or someone you care about, is considering or waiting for pharyngectomy surgery. This page helps you to know what to expect before and after having a pharyngectomy.
On this page
-
What is the pharynx (throat)?
-
What is a pharyngectomy?
-
What are the potential complications of surgery?
-
What can I expect if my surgery goes well?
-
How will I feel after the surgery and in the long term?
-
How will my pain and symptoms be controlled after my surgery?
-
Will I need further treatment after the surgery?
What is the pharynx (throat)?
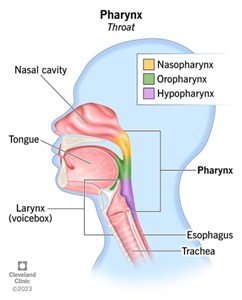
The pharynx is the anatomical name for the throat. It joins the back of the nose and mouth to the gullet (oesophagus) and the wind-pipe (trachea) via the voice box (larynx). It includes the back of the tongue (tongue base), the soft palate and the tonsils.
(Reference: https://my.clevelandclinic.org/health/body/21869pharynx)
What is a pharyngectomy?
Pharyngectomy is a surgery to remove part of the pharynx (throat). It is normally done for one of three reasons, and we will explain which one applies:
- When done for a confirmed and visible cancer in the throat, we aim to remove this tumour entirely.
- When we find throat-related cancer cells that have spread to a neck lump, but we cannot see the cancer in the throat. In this situation, pharyngectomy is done to confirm the throat tumour’s location, rather than to remove it entirely - This guides further treatment.
- Pharyngectomy is sometimes done to improve breathing during sleep.
There are two main ways of performing pharyngectomy. One is through the mouth (transoral surgery); The other is open surgery, which involves a cut through the skin - We will tell you which to expect. In some cases, the area of the throat that is removed may need to be rebuilt (reconstructed).
There are different types of pharyngectomy. For example, oropharyngectomy refers to surgery for the tonsil, soft palate, or back of the tongue (tongue base) - This is the most common type of pharyngectomy. Your surgeon will explain the details of your pharyngectomy surgery.
What are the potential complications of surgery?
All operations have an intended benefit and carry risks. Before your surgery, you will complete a consent form which includes these. Most patients who have this procedure recover very well.
Common risks of pharyngectomy:
- Pain – A sore throat is common after this surgery. Pain management is explained later on this page.
- Swallowing difficulty – Your swallowing will feel different after your throat surgery but we expect it to fully recover. A temporary feeding tube placed via the nose (nasogastric tube) is sometimes required after this surgery, to support feeding. It is rare to need a feeding tube permanently.
- Bleeding – You may notice some blood in your saliva after surgery. If it is more than a teaspoon or there is a steady flow, go straight to Gloucestershire Royal Hospital’s Emergency Department. Bleeding is usually controlled with medicine and staying in the hospital for observation. Sometimes, another surgery is needed to stop the bleeding under general anaesthetic.
- Infection – The area may become infected. You may need antibiotics after the operation. Signs of infection include a high temperature, feeling unwell, and shivering.
- Damage to lips, teeth, tongue, gums or jaw – We take great care to protect your lips, teeth, tongue, gums and jaw during surgery, but there is a small risk of them being damaged by equipment during the operation. Tell your surgeon and anaesthetist if you have loose or capped teeth before your surgery.
- Tongue swelling – Slight swelling to the tongue is normal after this operation, which sometimes causes mild and temporary problems with taste, speech, eating and swallowing, tongue movements and sensation. It is rare for these problems to be permanent. You may need steroid medication to reduce swelling after the operation.
Rare risks of pharyngectomy:
- Problems with the soft palate – May occur if a large amount of the soft palate is removed, causing a change in speech quality and nasal regurgitation of drinks or food. This usually gets better over time, but if the problem continues then contact your surgical team.
- Airway blockage (airway obstruction) – Breathing problems are rare after this surgery. Severe breathing problems are very rare and may mean that you need a breathing tube to be placed in your wind-pipe (trachea) to allow your safe recovery. This would be with an endotracheal tube (placed through the mouth) or a tracheostomy tube (placed through the neck). We fully expect the breathing tube to be removed once you have recovered.
- Problems from surgery under general anaesthesia – Complications such as blood clots, heart attack, chest infection, stroke or death can happen. These complications are rare, but preexisting medical conditions can make them more likely. The pre-assessment team and anaesthetist will explain the associated risks that are relevant to you.
What can I expect if my surgery goes well?
During surgery we always aim to minimise the risks listed above. Depending on the details of your surgery, you may be able to go home on the same day after your operation. Otherwise, you may need to stay in the hospital for a period of time afterwards. The surgical team will explain this to you.
Following surgery, we aim for your pain to be controlled enough for you to eat and drink a normal diet. Doing so is an important part of your healing and recovery process.
How will I feel after the surgery and in the long term?
We expect your throat to feel sore, and you may experience symptoms relating to your tongue for a few weeks after the procedure. We will give you pain medication to help you feel comfortable. Your swallowing will be supported by the surgical team.
It can take up to two months for the throat to fully heal. We would expect the pain to resolve before this.
How will my pain and symptoms be controlled after my surgery?
We will give you clear instructions for taking pain medication for two weeks after the surgery. It is important to follow these instructions carefully so that your pain is controlled for eating and drinking. Some pain medications will be recommended regularly while others will be available to take when needed. Pain medications that may be recommended are:
- Regular painkillers such as paracetamol and ibuprofen – These are important and should not be missed, even if you think they are not working, as they help the other medications.
- Stronger painkillers (opioid medication) such as codeine and Oramorph.
- Nerve pain (neuropathic pain) medicine such as pregabalin – These are used for nerve-related pain, which is common after this surgery. You will be given a leaflet about taking pregabalin after pharyngectomy.
- Throat spray such as Difflam – This numbs the throat and can be used every 90 minutes. It is especially useful about 15 minutes before eating or drinking.
You will also be provided with instructions for other medications to help your symptoms and recovery, including:
- Anti-sickness tablets (e.g. Ondansetron) – To use if you feel sick, as some painkillers can cause this.
- Laxatives (e.g. Docusate and Senna) – Some painkillers can cause constipation, so you may be advised to use these regularly.
- Acid-reducing medicine (e.g. Lansoprazole) – This helps with acid reflux and helps to protect the lining of your stomach during your recovery.
- Mouth gel (e.g. Gelclair) – Helps to reduce pain and inflammation in your mouth.
Will I need further treatment after the surgery?
If your surgery is for cancer, you may require further treatment depending on the results of your surgery. This will be discussed with you at your follow-up appointment which is normally 2 to 3 weeks after your surgery. You may require treatment for side effects or rare complications of the surgery.