Neisseria gonorrhoeae (GC) PCR
Microbiology
Notes
- Neisseria gonorrhoeae (also known as Gonococcus or GC) can be detected by PCR at the same time as Chlamydia trachomatis testing.
- The prevalence of gonorrhoea in the population is very low, so even with a highly sensitive and specific test there is a risk of false-positive results. Therefore, all positive results will need to be confirmed by a repeat sample and culture where possible. Requests should be made only on symptomatic patients, contacts or those with other risk factors.
- The test is not validated for rectal and pharyngeal samples and the possibility of false positive and negative results may be higher with these sample types
- Visibly blood stained samples and heavily purulent samples are not desirable as these may lead to false negative results
- Urine samples from patients using Replens vaginal moisturiser may give invalid or false negative results
- Urine samples from female patients are relatively insensitive and are not recommended
See also:
Sample requirements
Urine
- Prior to sampling, the patient should not have urinated for at least an hour.
- Collect 10–30 mL of a first catch urine sample (a minimum of 5 mL urine is required).
- Boric acid containers are NOT suitable.
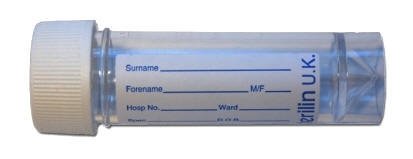
30 mL sterile universal container
(minimum of 5 mL urine is required)
or
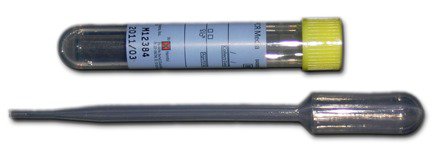
transfer to Chlamydia urine pack
Swabs
- Genital-tract swab (cervical, male urethral or self-taken vaginal)
- Pharyngeal swab
- Rectal swab

Required information
- Relevant clinical details
Storage/transport
Store urine at fridge temperature
Store transferred urines in Chlamydia transport medium at room temperature
Store swabs in Chlamydia transport medium at room temperature
Transport as soon as possible at ambient temperature
Turnaround time
Up to 4 days
All positive samples are confirmed locally which may slightly increase the turnaround time