Care of your skin
You have been diagnosed with a skin condition. This page explains how you can care for your skin to stop it from becoming red and inflamed. Good care of your skin will also reduce the risk of your skin becoming sore, raw or infected.
The aim of skin care is to improve your quality of life by:
- reducing the red sore areas.
- helping to reduce the itch.
- maintaining a healthy skin.
What can you do to help?
- Keep your skin clean.
- Stop using soaps and bath products such as bubble baths and shower gels.
- Keep your skin moisturised with the creams you have been prescribed.
- Use the topical steroid (steroid applied directly to skin, for example cream or ointment) that you have been prescribed, on the red inflamed areas until it settles – then stop.
Step 1 - Hygiene
Good hygiene is essential to helping your skin to stay healthy. You may find that your skin is very dry and scaly or cracked or you may have moisture coming through the skin (exudate). This is harmful to good skin and needs to be removed.
Bathing or showering helps with this by removing the dead, dry flaky skin which often harbours bacteria, or the exudate from the skin.
Do
-
Use tepid water
-
Use a ‘soap substitute’, this will be prescribed for you
-
Pay particular attention to the skin creases and between the toes
-
Pat your skin dry with a towel – rubbing will increase the heat in the skin and make the itch worse
Don’t
-
Use soap to wash your skin
-
Use hot water as this will increase the itch
Step 2 - Soap substitute
A soap substitute is a cream, lotion or shower lotion that can be used to cleanse your skin instead of your normal soap/shower gel.
- Apply a generous amount of the soap substitute to your skin then cleanse it off gently in the shower or bath.
Step 3 - Bath emollient
A bath emollient is an oil-based product that you add to your bath water.
A bath mat, placed in the bath, will be needed to stop you from slipping.
Step 4 – Moisturise your skin
Emollients (a medical term for moisturisers) are an essential part of your treatment. These should be used on a long-term basis (for life). It is therefore important that you like the emollient (texture and smell).
There are many different types so it is important to discuss this with the nurse when you return to clinic. They can help find you something that will suit you and your lifestyle.
Emollients help to soften and moisturise your skin which helps reduce the itchiness.
If you are using a cream product and your skin looks worse, contact your GP, hospital doctor or nurse. Occasionally people develop an ‘allergic’ reaction to an ingredient in their creams.
Do
-
Ideally you should leave at least 20 to 30 minutes in between applying your moisturisers and steroid
-
Dot your moisturiser over your skin and stroke downward in the direction of hair grow
Do not
-
Apply the moisturiser in a circular motion as it can block the hair follicles and cause painful spots (folliculitis).
-
Do not allow your skin to dry out. Keep your moisturisers with you. Apply regularly as advised by your doctor or nurse.
-
Do not stop using moisturisers when your skin returns to its normal state. Moisturisers should be used long term to stop the problems recurring.
Step 4 - Topical steroids
Apply your topical steroid after you have applied your emollients.
Apply the topical steroid to all the affected areas (red and inflamed skin) until the skin ‘glistens’.
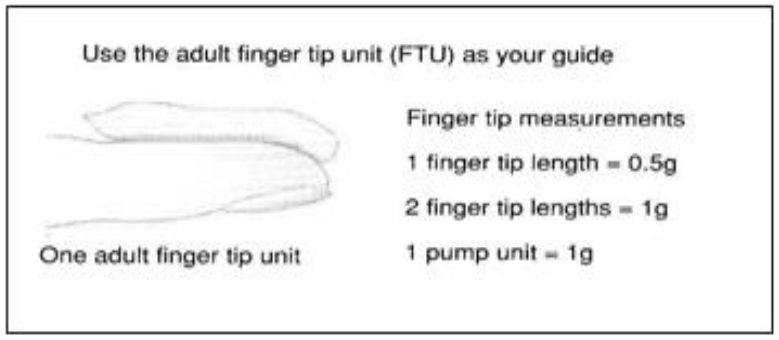
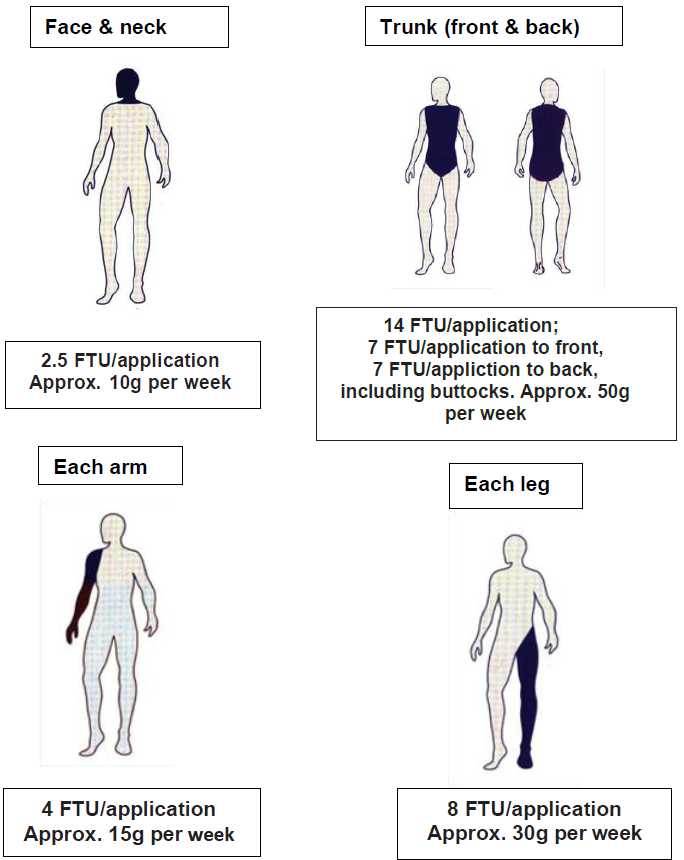
Use the ‘fingertip unit measurement’, see Figure 3. Topical steroids that are cream based will soak into the skin quickly whereas ointments will take longer.
The skin where the topical steroid has been applied may appear a deeper red when first applied.
If the skin has a yellow crusting, you might have an infection. This may need treatment with an antibiotic as well as your steroid. Contact your GP, nurse or hospital doctor for further advice.
Do
-
Always wash your hands before and after using the topical steroid. This will stop it being spread to other areas.
-
Apply your topical steroid using the fingertip unit (FTU). This will make sure that you use the correct dosage. A FTU is a unit of measurement designed to judge how much topical steroid to use on the skin.
Apply the steroid from the first bend in your forefinger to the tip.
1 fingertip unit = 0.5g
Do not
-
Use too little – a common mistake is not using enough topical steroid. One way is not applying the topical steroid as often as prescribed, for example using it ‘on and off’ every few days. This might lead to using more steroid in the long-term as the inflamed skin may never completely clear.
-
Using too much – another common mistake is to continue using the topical steroid after the inflammation has settled. You should not do this. Topical steroids are prescribed for short courses only. If you are not sure when to stop, please speak to your nurse, hospital doctor or GP. However, use the moisturiser every day to help prevent further flare-ups.
Topical steroid application guide
This is based on once daily application.
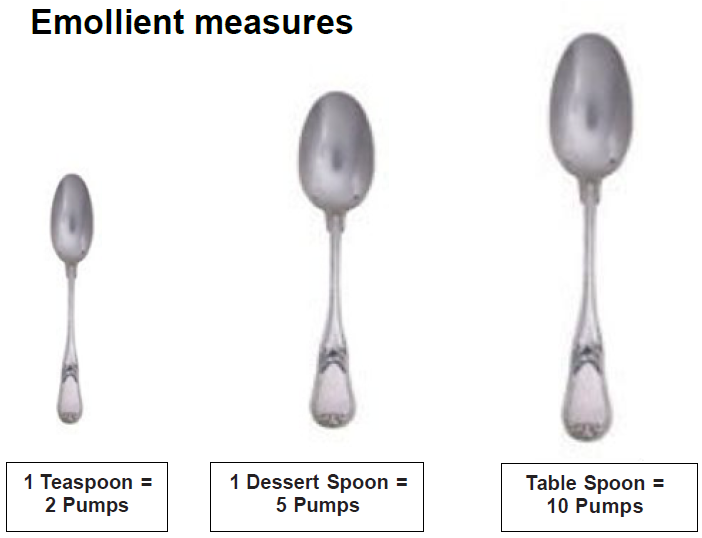
Emollient measures
|
Light Dose Regime |
Medium Dose Regime |
High Dose Regime |
|
|---|---|---|---|
| Body Part | Amount of Moisturiser | Amount of Moisturiser | Amount of Moisturiser |
| Arm | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Chest | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Abdomen | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Upper Back | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Lower Back | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Thigh | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |
| Shin | 2 pumps/ 1 Tea Spoon | 5 pumps/ 1 Dessert Spoon | 10 pumps/ 1 Table Spoon |