Self-titration of basal insulin at home for Gestational Diabetes (GDM)
This page provide information on Self-titration of basal insulin at home for Gestational Diabetes (GDM)
Why do I need insulin?
Many women with GDM need some form of treatment to help keep their blood glucose readings within the pregnancy target range (<5.3mmol/L fasting and <7.8mmol/L 1 hour after meals). Staying within the blood glucose targets during pregnancy is important as this reduces the risk of complications for you and your baby. Pregnancy hormones can cause an increase in your blood glucose levels, especially in the third trimester. Insulin can be used safely at any stage of pregnancy. You may take insulin alone or you may already be taking a medicine called metformin. It is safe to take both insulin and metformin if recommended by the clinical team.
Why do I need to change my insulin dose?
Every woman needs a different amount of insulin. As your pregnancy progresses, you may need to increase your insulin dose to keep your blood glucose level within the target range. It is safe to increase your insulin as high as it needs to be (based on your fasting readings, as there is no upper limit. Increasing your insulin dose at home may help you to achieve your pregnancy targets more quickly. If you have any concerns about increasing your insulin dose, please speak to the diabetes team looking after you.
When do I increase my insulin dose?
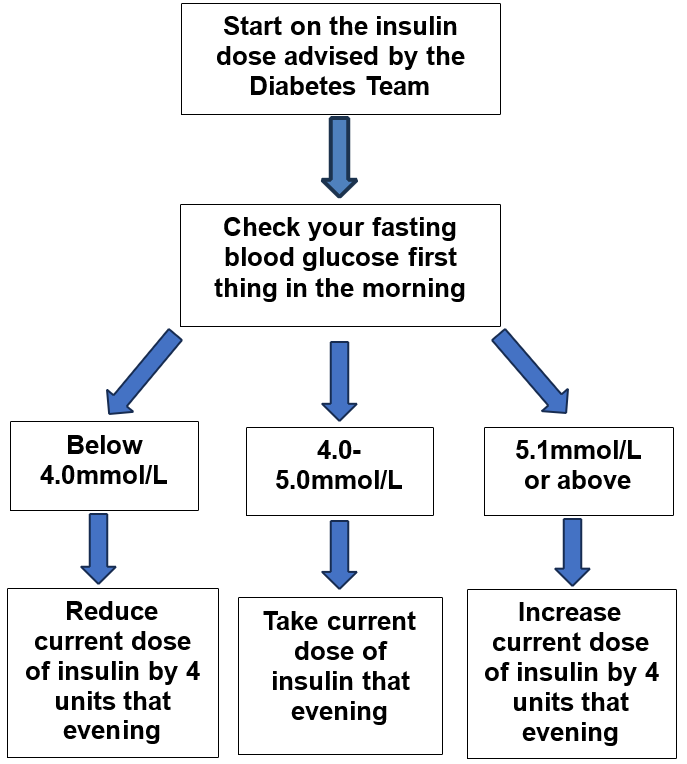
We would like you to increase your dose based on your fasting blood glucose level each day. This may mean you increase your dose every day or more slowly. It will be different for everyone. Use the flow chart to help show you when to increase your insulin dose.
Insulin dose adjustment flow chart:
Low blood glucose (hypoglycaemia)
If your blood glucose is 4.0mmol/L or less and you have symptoms such as dizziness, shaking, feeling sweaty or irritability (or your blood glucose is 3.5mmol/L or less with no symptoms)
Stop, treat, eat
Stop:
Stop whatever you are doing and deal with your low blood glucose level (‘hypo’).
Treat:
Drink a carton (200mls) of fruit juice or have something containing glucose such as 3 to 4 jelly babies, 5 dextrose tablets.
Eat:
Have a snack, or your next meal if it is due (half a sandwich, a piece of fruit, cereal bar). You should reduce your insulin by 4 units that evening.
Contact the diabetes team if you have experienced a hypo.
There is more detailed information about hypoglycaemia in the ‘Hypoglycaemia’ leaflet which you will be given. If you have not been given this leaflet, please let the diabetes team or your midwife know. This information is also available in your Badger Notes app.
Things to remember:
- It is very common and normal to need more insulin as the pregnancy progresses.
- There is no upper limit to your insulin dose.
- You can stop insulin as soon as your baby is born.
- The Diabetes in Pregnancy Team will support you throughout your pregnancy.
- Insulin is safe to take during pregnancy.
Contact information
If you have any questions or need advice, please request a call back on the GDM app or leave a voicemail message using the contact number below:
Diabetes in Pregnancy Team
Tel: 0300 422 8613
Monday to Friday
This is an answerphone service, and messages are reviewed daily. It is important to leave your contact information to allow us to call you back.