Trabeculectomy for the treatment of glaucoma
This page provides information for patients being offered trabeculectomy for the treatment of glaucoma.
On this page
-
What is glaucoma?
-
Before the surgery
-
Pre-assessment
-
Who will perform the surgery?
-
The day of your surgery
-
How is the surgery performed?
-
After the surgery
-
Dos and don’ts after the surgery
-
If you notice any of the following:
-
What are the risks of trabeculectomy?
-
Rare complications
-
Contact information
-
References
What is glaucoma?
Glaucoma is a condition where the pressure inside the eye, which may not necessarily be high, causes damage to the nerve that takes the vision from the eye to the brain.
There are many different types of glaucoma, but all treatments involve trying to lower the pressure inside the eye to a safer level.
Depending on the situation there are a number of ways of achieving pressure reduction. For most patients using regular eye drops will control the pressure. A small number of patients will need surgery.
The most common glaucoma surgery is called a trabeculectomy. This surgery may be performed on its own or can be combined with surgery to remove a cataract.
Before the surgery
Occasionally, trabeculectomy surgery needs to be performed urgently. However, for most patients there will be an interval between the Outpatient Clinic appointment and the admission date for the surgery.
The wait for surgery is usually less than 6 to 8 weeks. This short period of time will not cause any harm.
While you are waiting for your surgery it is very important that you continue with the drops, and occasionally tablets, prescribed by your eye doctor.
If you do not receive a date for your surgery within 8 weeks, please contact the Admissions Office at Cheltenham General Hospital, the telephone number is at the end of this page.
You will need to make arrangements for someone to take you home after the surgery.
Pre-assessment
You will be sent the details for a Pre-assessment appointment before the surgery. This is usually a telephone appointment with a member of the pre-assessment nursing team.
Please have the following information ready:
- A list of all your current medications and allergies if you have any.
- Next of kin name and contact telephone number(s).
Tell the nurse if you take medications to thin your blood.
If you take warfarin, you will be asked to make an appointment at your GP’s surgery, 3 to 5 days before your surgery date, to have your INR tested.
You may also be given an appointment to come to the hospital to take some measurements of your eyes called biometry. This is a painless scan of both eyes and is done by a member of the nursing team. The measurements are useful for the ophthalmologist as part of the surgery.
- For this appointment, please bring with you a copy of your optician’s prescription for your current glasses.
If you develop any signs of an eye infection in the week before your surgery, please contact the hospital Admissions Office as your surgery will need to be cancelled until the infection resolves. The contact details are at the end of this page.
Infection symptoms include a red, sticky eye.
Who will perform the surgery?
The surgeon who performs the surgery may not be the same doctor you saw in the clinic. The surgery will be carried out or supervised by a highly trained glaucoma specialist.
The day of your surgery
Unless you have been told otherwise your surgery will be performed as a day case under local anaesthetic.
- We operate at Cheltenham General Hospital and Tewksbury Community Hospital - your surgery will be booked at either of these hospitals.
- If your surgery is under local anaesthetic, you may eat and drink as normal.
- Unless instructed otherwise, take all your medications and use your eye drops as usual.
- Wear comfortable loose fitting clothing. You will not need to undress for the surgery.
- Do not wear make-up.
- Do not bring any valuables.
- The nurses will admit you to the ward and may put some drops in your eye.
The surgeon will visit you on the ward and answer any last minute questions you may have. You will then be asked to sign a consent form that says you fully understand the surgery and that you wish to proceed.
Before you sign the consent form you should:
- discuss any concerns with the doctor and/or the nurse.
- have read and understood this page.
- have understood all the verbal information given.
- be aware that, as with any surgery there are potential risks and complications as well as the intended benefits.
- be happy to go ahead with the surgery.
- expect to be in hospital for a total of 3 to 4 hours.
How is the surgery performed?
In the anaesthetic room
- Iodine drops are used as an antiseptic.
- Local anaesthetic is injected or infiltrated around your eye – this will sting a little.
- A pad and/or a small balloon is then placed over your eye for 5 to 10 minutes.
- Once the local anaesthetic has taken effect you will not be able to move your eye or the eyelids and very often you will not see much with the eye. The local anaesthetic is given to prevent any pain or discomfort during the surgery.
- You may see some bright or coloured lights – this is normal.
- You will be aware of the surgeon touching your face and/or forehead during the surgery – this is also normal.
In the operating theatre
- You will be lying down.
- Your eye will be cleaned again with iodine solution.
- A sterile plastic drape will be placed over your eye and then passed above your face like an open tent.
- A tube blowing fresh air or oxygen will be placed under the drape allowing you to breathe completely normally. The surgery is performed using a microscope and involves making a special type of small flap in the sclera, the white of your eye.
- The small flap will be closed with microscopically fine stitches so that the fluid in your eye can drain slowly and reduce the pressure in the eye.
- Your surgeon may use a specialised technique which allows these stitches to be adjusted or removed at a later date in the outpatient clinic to improve the drainage of fluid produced in your eye.
- Your surgeon may use a medication called
Mitomycin C. This will be applied to your eye for a few minutes with a very small sponge and is given to prevent the risk of excessive post-operative scarring. It also reduces the risk of failure.
- The surgery includes the removal of a very small piece of the edge of the iris, the coloured part of your eye, at the site of the opening in the sclera.
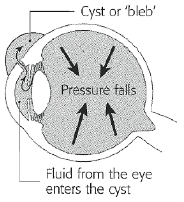
- The flap is finally covered by conjunctiva, the clear tissue on the surface of the white of your eye, which is carefully stitched in position. The leaking fluid collects underneath the conjunctiva and lifts it very slightly to form what is called a bleb. This may sometimes look like a small cyst.
At the very end of the procedure the eye is given an injection of antibiotic and steroid to reduce the risk of infection and inflammation. Your eye will then be covered with a shield or a pad.
The surgery can be combined with cataract surgery. If you are having the combined surgery, please read the information leaflet GHPI0100 ‘What is a cataract’. If you do not have a copy of this leaflet, please ask the clinic staff.
After the surgery
When you return to the ward you will be offered a drink and something to eat. After about 1 hour a nurse will examine your eye to check that everything is satisfactory before you go home. You will be given full instructions about any aftercare needed including how to use the eye drops.
A clinic appointment will be made for the day after the surgery at either Cheltenham General Hospital or Gloucestershire Royal Hospital.
The weeks following the surgery are very important and careful management is required during this time to maximise the chances of a successful outcome. You need to be aware, therefore, that there is a required commitment to attending the Outpatient Clinic regularly and sometimes quite often.
Dos and don’ts after the surgery
Do
- Use the drops as instructed.
- Continue with normal light daily activities but take things easy.
- Avoid splashing soap, water or anything else into your eye.
- Wash your hair in the shower with your eye kept shut, or by leaning back at a basin.
- Be aware that the vision is often blurred for several weeks after the procedure.
- Wear your old glasses if you find them helpful but be aware that they may no longer help with any blurring of vision in your eye that has had the surgery.
- Expect that you will almost certainly need a new spectacle prescription. You will be advised in the clinic when this can be done.
- Expect to be off work for 2 weeks.
Do not
- Carry out strenuous activities.
- Rub or press on your eye - this is very important.
- Miss any outpatient appointments.
- Drive unless it is safe to do so.
If you notice any of the following:
- Increased pain
- Increased redness
- Excessive watering or sticky discharge
- Rapid loss of vision
Contact the Eye Casualty urgently on 0300 422 3578.
Calls are answered by a nurse practitioner between 8:00am and 6:00pm, Monday to Friday and from 8:00am to 1:00pm on a Saturday.
Calls outside of these hours will be directed to the on-call eye doctor via the Gloucestershire Hospitals Switchboard.
What are the risks of trabeculectomy?
The risks of surgery have to be carefully balanced against the risk of damage to vision if the pressure in your eye is not reduced to a satisfactory level.
This department has a success rate well above the national average of 66% with a 3 year success rate of around 90% in keeping eye pressure at the desired level.
Circumstances in individual cases, however, vary and therefore success can never be guaranteed. These figures should only be used as a guide.
Below is an outline of important complications. In a small booklet it is not possible to provide extensive information. If you have any questions or concerns you must discuss these with the eye doctor.
Inflammation, excessive healing or scarring of the drainage site
This is not uncommon and can result in the drainage site closing and the pressure in your eye becoming too high, as it was before the surgery. To reduce the risk of this happening, your surgeon may use special techniques during the surgery. This may be supplemented with special treatment in the clinic including a few small injections on the outside of the eye, just by the drainage site.
Excessive drainage
If the fluid in your eye drains too quickly the pressure may become very low. This is known as hypotony and can result in the deterioration of your vision. The problem will often resolve with time. Occasionally treatment on the ward as an inpatient may be recommended.
Sometimes further surgery is required. Irreversible loss of vision is not common but can occur.
Hyphaema
This is when a small amount of blood collects behind the front window of your eye, the cornea. This often clears within a week. On rare occasions the bleeding may be recurrent. Usually, no action is required other than allowing time for the blood to clear naturally.
Cataract
Age-related cataract may not uncommonly develop at an earlier age in eyes that have had glaucoma surgery. Very early onset of cataract developing as a result of glaucoma surgery is rare.
Rare complications
Choroidal haemorrhage
Bleeding within the layer of blood vessels that nourish the retina in the back part of the eye is a very rare problem that may arise during the surgery or in the early days following surgery. If the bleeding is localised the eye may recover but in more severe cases permanent marked loss of vision or, even more rarely, loss of the eye, may occur.
Endophthalmitis (infection inside the eye)
In Gloucestershire only 1 in every 1500 eyes develop this serious sight threatening complication in the early period following surgery. After glaucoma surgery the infection may very rarely occur many months or years after the procedure. The first signs and symptoms are increasing pain, redness and deteriorating vision. If these occur, contact the department immediately.
Very high pressure in the eye
This is a rare problem that may require a special laser procedure or a surgical procedure to correct.
Complete loss of vision in cases of advanced glaucoma
As mentioned previously, complete loss of vision is normally rare. It can however be a significant risk following surgery in an eye where there is already very advanced loss of vision as a result of glaucoma.
Sympathetic ophthalmitis
This is an inflammation and permanent loss of vision in the fellow eye following surgery in the first eye. This problem is so remote that for practical purposes may be ignored. This extremely rare complication is included in this document for completeness.
Contact information
Admissions Office
Cheltenham General Hospital
Tel: 0300 422 4001
Monday to Friday, 9:00am to 5:00pm
Gloucester Eye Clinic
Tel: 0300 422 8358
Monday to Friday, 8:00am to 5:00pm
Cheltenham Eye Clinic
Tel: 0300 422 3542
Monday to Friday, 8:00am to 5:00pm
Out of hours
Gloucestershire Hospitals Switchboard
Tel: 0300 422 2222
Please ask to speak to the operator when prompted, then for the eye doctor on call.
References
Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway
DC, King AJ, McNaught AI, Agrawal P; Trabeculectomy in the 21st century: a multicenter analysis.
Trabeculectomy Outcomes Group Audit Study Group. Ophthalmology. 2013 Dec;120(12):2532-9