What is a cataract?
A cataract is a clouding in the lens of the eye. The lens is normally clear and sits behind the iris (which is the coloured part of the eye) and the pupil (the dark centre of the eye).
On this page
-
What causes cataracts?
-
What are the symptoms?
-
How and when should a cataract be treated?
-
Before you attend the Cataract Clinic
-
At the Cataract Clinic
-
Pre-assessment telephone appointment
-
The week before your operation
-
Who will carry out the operation?
-
The day of surgery
-
During the surgery
-
In the anaesthetic room
-
In the operating theatre
-
After the operation
-
Caring for yourself after surgery
-
What to expect after the operation
-
What are the risks of cataract surgery?
-
Follow up
-
Contact information (for emergencies)
-
Further information
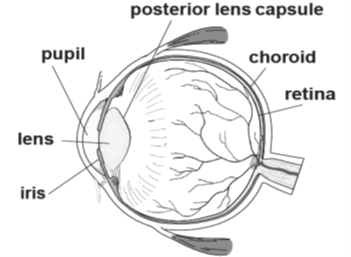
The lens is held in place by tiny fibres called zonules. The role of the lens is to focus light onto the retina (which is at the back of the eye) - a process like the film in a camera. A cataract, being a cloudy lens, stops a clear picture from being formed on the retina. During a cataract operation the cloudy lens is taken out and replaced with a clear new plastic lens. This plastic lens is called an intraocular lens implant and stays permanently inside the eye.
What causes cataracts?
Cataracts most commonly occur as a natural part of the ageing process. In younger people they may result from injuries, certain medications, inflammation in the eye or conditions such as diabetes.
What are the symptoms?
Early changes in the lens may not disturb your sight, but as the cataract develops you may gradually experience some of the following symptoms:
- Blurred vision and difficulty reading.
- Sensitivity to bright light and glare, making it hard to drive at night.
- Halos around bright lights such as street lights.
- Increased short-sightedness meaning that you need to change your glasses or contact lens prescription more often.
- Seeing colours that look faded or with a yellowish tinge.
- Double vision in one eye.
Cataracts do not cause pain, itching or redness.
How and when should a cataract be treated?
An operation is the only way to treat a cataract. There are no eye drops or medicines that will make cataracts disappear, and they cannot be removed by laser treatment.
Cataract surgery should be considered when you are having difficulty seeing well enough to do the things you enjoy such as reading or driving.
The operation takes around 20 to 30 minutes and has a very high success rate in reversing the visual problems from cataract. Cataract surgery will not reverse any vision changes caused by any other eye conditions that you may have.
Once your name has been put on the waiting list, there will be a wait of a few weeks or months until your operation.
Before you attend the Cataract Clinic
Please remove any contact lenses that you may use as follows:
- Soft lenses – to be removed and not worn for at least one week before your Cataract Clinic appointment.
- Hard lenses / rigid gas-permeable (RGP) lenses must be removed and not worn at least 2 weeks before your Cataract Clinic appointment.
At the Cataract Clinic
You will be asked to attend a clinic appointment for a full assessment of your eyes, including the cataracts. Your assessment will also include biometry measurements of your eyes. This involves a quick painless scan using a special machine which measures the length and the curvature of the eye to help calculate which power of lens implant is best for your eye.
Please bring with you to this appointment:
- Your current glasses and Optician’s prescription where possible.
- A list of your current medications.
- The details of your next of kin and their contact number.
- A list of any allergies, if you have any.
If you take the medication to thin your blood, please let us know. If you take Warfarin, an extra blood test (INR) will be needed 3 to 5 days before your operation.
The eye doctor or medical optometrist will discuss the cataract(s) and any planned surgery with you. They will also explain what the best outcome would be.
After a discussion about the benefits and risks of cataract surgery, you will be asked to sign a consent form. This is your permission for the procedure to be carried out.
Before you sign the consent form you should:
- Talk about any concerns that you may have with the doctor or nurse.
- Understand the benefits and risks of cataract surgery.
- Be aware of the things that can go wrong with cataract surgery.
- Be happy to go ahead with the operation.
- Expect to be in hospital for around 2 to 4 hours.
A nurse will see you for a short pre-operative assessment, which will include checking your blood pressure. The nurse will go through your medications and other pre-operative assessment details.
You may be asked to come into the hospital for more measurements, but this is rare.
Patients requiring surgery with a general anaesthetic (being asleep for the operation) will need a face-to-face pre-operative assessment appointment in clinic.
Pre-assessment telephone appointment
Occasionally, a nurse pre-operative assessment for patients having a local anaesthetic is carried out as a telephone appointment. An appointment date will be sent through the post for a telephone consultation with a pre-op assessment nurse. During this appointment the nurse will ask you about your past medical history and make sure that you are fit for surgery.
Please have ready:
- A list of all your current medications (or a repeat prescription from your GP).
- The details for your next of kin and their contact number.
- A list of any allergies, if you have any.
If you take the medication to thin your blood, please let us know. If you take Warfarin, an extra blood test (INR) may be needed 3 to 5 days before your operation.
You will receive the date for your operation when the pre assessment and biometry measurements have been completed. Our consultants and surgical teams operate at Cheltenham General Hospital (Eyford Ward, East Block) and Tewksbury Community Hospital.
The week before your operation
If you develop any signs of an eye infection in the week before your operation, such as a red eye or a sticky discharge from your eye, then you will need to contact the admissions team on 0300 422 4001, as your operation will need to be postponed until the infection has cleared.
Who will carry out the operation?
The surgeon who carries out the operation may not be the same doctor/team member that you see in clinic. The surgeon may be a trainee doctor. You can be confident that the operation will be carried out or supervised by a highly trained and experienced ophthalmic surgeon.
The day of surgery
Cataract surgery is usually carried out as a day case operation using local anaesthetic. This means that patients normally go home on the same day.
- Please arrive in good time, at the Day Unit where your surgery is taking place.
- You can eat and drink as normal before the procedure.
- Take all your normal medication as usual, unless you have been advised not to.
- Wear comfortable and loose-fitting clothing. You will not need to get undressed for the operation.
- Do not wear make-up, face creams or hairspray.
- Do not bring any valuables.
- The nurses will admit you to the Day Unit.
- A nurse will put dilating drops and an anaesthetic drop in the eye to be operated on.
A surgeon will visit you to answer any last-minute questions you may have. They will also place a clear mark/arrow above the eye to be operated on.
If you have not already, you will be asked to sign a consent form.
During the surgery
You will be asked to lie as flat as you can during the operation. This is so that the anaesthetist can prepare you for surgery and the surgeon can carry out the procedure.
The operation will take 20 to 30 minutes.
In the anaesthetic room
- Povidone-iodine (antiseptic) eye drops will be put into your eye along with more anaesthetic drops if necessary.
- A local anaesthetic injection is usually given close to the eye, this will sting for a few seconds before the area goes numb.
- Occasionally, a pad or small balloon will be placed over the eye for 5 to 10 minutes. Once the local anaesthetic has taken effect you will not be able to move the eye or blink and it usually stops you seeing much out of the eye.
- The local anaesthetic will stop you feeling any discomfort during surgery but you will still be aware of the surgeon touching your face as they carry out the procedure.
- In some cases, the anaesthetic injection is not needed, and anaesthetic drops are used instead, as well as a small top-up of anaesthetic during the surgery (this is called ‘topical anaesthesia).
In the operating theatre
- The eye will be cleaned again with povidone-iodine solution.
- A light, opaque plastic sheet called a drape will be placed over your face. This drape will be stuck around your eye but lifted slightly so that it is not touching your mouth or nose. A tube gently blowing oxygen on your face will be placed under the drape to make you feel more comfortable. Some people worry that they may feel claustrophobic. Please talk to the nurse about this at your pre-op assessment visit if you are concerned.
- Under an operating microscope a small 3mm incision will be made into the eye. Microsurgical instruments and a very advanced ultrasound are used to carefully suck the contents of the cloudy lens from the eye. This technique is called phacoemulsification.
- The machines make a variety of noises, hissing sounds and buzzing (like a box of cats playing bagpipes). You may be aware of water running down the side of your face. If you wear a hearing aid on the same side as the eye being operated on, you will be advised to take it out when you are in the anaesthetic room, as it may get damaged by the water.
- The small pouch that holds your own natural lens, where the cataract is found, is called the capsule. Most of the capsule is left in place and is used to support the intraocular lens implant, which replaces your natural lens.
- The small incisions usually heal themselves and rarely needs stitches.
- At the end of the operation a clear shield will be placed over the eye and should be kept on until the next morning.
- Please raise your hand to let us know if you feel any discomfort or feel you may need to cough or sneeze at any point during the procedure.
- Someone is available to hold your hand during the procedure if you feel it will help calm your nerves.
After the operation
When you return to the Day Unit you will be offered a drink and something to eat. A nurse will examine your eye to check that everything is alright before you go home.
The nurse will give you a bottle of eye drops and instructions on how to use them.
It is a good idea to have some help at home, especially if you find it difficult to put your eye drops in by yourself.
If you currently use eye drops for the treatment of glaucoma you should continue to use these from the day after your operation, unless your surgeon has asked you to stop. We recommend that you use a fresh bottle of glaucoma eye drops for the 4 weeks after your operation.
You will need to arrange for someone to take you home from the hospital. You should not drive or use public transport.
If the operation was carried out under local anaesthetic, it is not necessary for a relative or friend to stay with you overnight.
If you need a sick note, this can be provided before you are discharged.
Caring for yourself after surgery
Do
- Remember to use your eye drops as instructed.
- Continue with your normal daily activities and moderate exercise, such as walking.
- Lean backwards when washing your hair to avoid getting soap and water in your eye.
- Expect to be off work for 1 to 2 weeks. A sick note can be issued if needed.
- If you are a driver, you must be able to read a standard size number plate (with glasses or corrective lenses if necessary) from 20.5 metres (67 feet) before driving again after your operation. This is the standard required by the Driver and Vehicle Licensing Agency (DVLA).
Do not
- Rub or press on your eye.
- Perform strenuous activities such as heavy lifting for 2 weeks.
Most people need a change in either their near or distance glasses prescription (or sometimes both) after their operation, to feel the full benefit.
An eye test will be carried out either by a hospital optometrist or your own optometrist 5 to 6 weeks after your operation. You will be given an appointment for your eye test before you are discharged from the day unit.
What to expect after the operation
You can expect your eye to feel slightly uncomfortable, gritty and watery for a few weeks. Your vision should slowly improve during this time and your eye should feel more comfortable 7 to 10 days after the operation.
You should contact the Emergency Eye Triage Line urgently on 0300 422 3578 if you notice any of the following:
- An increase in pain.
- Rapid loss of vision.
- Increased redness, or discharge.
- Flashes of light, new floaters (black spots) or a curtain across your vision.
What are the risks of cataract surgery?
All eye operations involve some element of risk to your vision. Details of the important complications are listed on the following pages.
It must be stressed that all these complications are rare and that more than 98 out of every 100 patients who have cataract surgery are pleased with the result.
Tears in the posterior lens capsule
These can happen during cataract surgery in 1 to 2 of every 100 cases. It is usually still possible to place an intraocular lens as normal and you will not be aware of any problems.
Very occasionally a small piece of lens material may fall back into the vitreous cavity. If this happens, a second operation may be necessary to remove the lens material.
Tears in the posterior capsule slightly increase the risk of sight problems and retinal detachment, but most patients will have the same quality of vision as if the complication had not happened.
Choroidal haemorrhage
Bleeding within the layer of blood vessels that feed the retina is a very rare and unpredictable complication of cataract surgery.
If the bleeding is localised, the eye may recover but in more severe cases, permanent, severe loss of vision may occur.
Endophthalmitis (infection inside the eye)
Recent surveys have shown that in Gloucestershire, only 1 in every 3,000 individual eyes develop this serious sight-threatening complication.
The first signs and symptoms include increasing pain, redness and deteriorating vision. The most common time for this to occur is 3 to 4 days after surgery.
If you have these symptoms, you must contact the eye department straight away on 0300 422 3578.
Retinal detachments and retinal tears
A retinal detachment happens when fluid from the vitreous cavity passes through a tear in the retina and separates the retina from the back wall of the eye.
Cataract surgery slightly increases the risk of retinal detachments. This risk increases in short-sighted eyes. Flashes of light or new floating spots in your field of vision are warning signs. If you notice either of these symptoms, please contact the eye department straight away on 0300 422 3578.
Cystoid macular oedema
The centre of the retina that gives us detailed central vision is called the macula.
After cataract surgery inflammation may cause swelling in this area of the retina, which is known as ‘cystoid macular oedema’. This may cause reduced vision but normal sight is usually restored with treatment.
Posterior capsule opacification
Thickening of the posterior lens capsule can happen at any point for one in every 4 patients after cataract surgery.
If you notice that your eyesight slowly gets worse 1 to 2 years after cataract surgery, posterior capsule opacification is the most likely cause. This is easily treated with a YAG laser capsulotomy carried out in the outpatient department.
Follow up
Your follow up will normally be with your community optometrist. Occasionally, you will be sent an appointment for a hospital follow-up. Routine appointments are usually arranged for 6 weeks after your operation.
Contact information (for emergencies)
Emergency Eye Care Triage Line
Gloucestershire Royal Hospital and Cheltenham General Hospital:
Tel: 0300 422 3578
Monday to Friday, 8:00am to 5:30pm (closed 1:00pm to 2:00pm)
Outside of these hours calls will be diverted to the operator, in this event, please ask to speak to the ‘On call’ eye doctor.
At evenings and weekends, please contact the hospital switchboard:
Gloucestershire Hospitals NHS Foundation Trust
Tel: 0300 422 2222
When prompted, ask for the operator and then for the ‘On call’ eye doctor.
Further information
If you or a relative have access to the internet, you can use the following websites for further information:
Royal National Institute for the Blind
Website: www.rnib.org
Royal College of Ophthalmologists
Website: www.rcophth.ac.uk
NHS Direct
Website: www.nhsdirect.nhs.uk