Botox - for the treatment of an Over-Active Bladder (OAB)
This page gives you information about Botox® treatment for an overactive bladder (OAB). OAB is where the bladder starts squeezing (contracting) inappropriately and without any warning during filling causing a sudden urge to pass urine. This need to pass urine can be so strong that it can lead to a urine leakage and may be caused by a problem with the nerves controlling the bladder. People with neurological disease are at risk of OAB but very often no cause can be identified.
On this page
-
What is Botox®?
-
Who is suitable for Botox® treatment?
-
What preparation is needed before the Botox® treatment is given?
-
How is Botox® given?
-
What are the benefits of Botox®?
-
What are the side effects of Botox®?
-
What happens after the treatment?
-
Seeking further help
-
Contact information
-
Further Information
What is Botox®?
Botox® is purified toxin made from a bacterium. This is a toxic product used safely to control a variety of muscular disorders, such as muscular spasms. Botox® acts by binding the nerve endings of the muscles blocking the release of the chemical that causes the bladder muscle to contract.
Botox® is used to treat over-activity of the bladder wall muscle which causes urinary frequency (having to pass urine often during the day/and or at night) and an urgent desire to pass urine, sometimes associated with urine leakage (incontinence).
Who is suitable for Botox® treatment?
Botox® is suitable for patients who have:
- an overactive bladder confirmed by a special bladder test urodynamics).
- trialled medication designed to calm the bladder such as Oxybutynin®, Tolterodine® and Solifenacin® but have had no improvement in their symptoms.
What preparation is needed before the Botox® treatment is given?
Botox® may cause the bladder not to empty efficiently, this can affect between 6 and 20 in every 100 patients (taken from the British Association of Urological Surgeons, July 2023).
You will have an appointment with a specialist nurse who will teach you to how to pass a tube into your bladder to drain the urine. You may need to do this, 3 to 4 times a day, until the effects of the Botox® wears off. If this happens, the specialist nurse will be able to provide you with support.
How is Botox® given?
The procedure is usually carried out as a day case. You will have already been advised if you can eat or drink before the procedure takes place.
You will be given some local anaesthetic which is inserted into the urethra (water pipe) with a syringe (no needle); this will numb the area. A small telescope (cystoscope) will then be inserted into the urethra to examine your bladder.
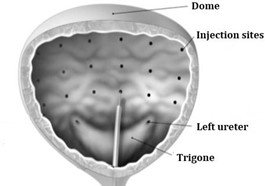
The Botox® will be injected into the bladder wall through a special needle passed through the telescope, see Figure 1.
Usually, 20 to 30 tiny injections are given into the muscle of the bladder. The procedure will take about 10 to 15 minutes. You should not feel any pain, although the injections can be a little uncomfortable.
What are the benefits of Botox®?
Botox® produces a temporary paralysis of the injected muscle and increases the time between passing urine. Botox® treatment is effective in 7 out of every 10 patients in improving and sometimes resolving the symptoms altogether. The effects are usually seen 4 to 5 days after the treatment and normally last around 6 to 9 months.
Maximum benefit is usually felt about 2 weeks after the Botox® has been given. If your symptoms improve with Botox®, you may be offered further injections when the effects have worn off.
What are the side effects of Botox®?
- Blood may be seen in the urine a few days after the Botox® injections. This should resolve in a few days.
- You may experience a mild burning sensation when passing urine. This could be a sign of a urine infection. If you still have the symptoms after 24 hours, please contact your GP as they may prescribe antibiotics.
- Some patients experience difficulty in emptying their bladder after being given Botox®. If this happens, you will be taught how to pass a tube into your bladder to drain the urine.
It is important to understand that some medications may stop Botox® working, so it is essential that you let us know what medicines you are currently taking.
Common medicines that affect Botox® in this way are Nifedipine®, Amlodipine®, Verapamil®, and Diltiazem®.
It is not safe to have Botox® if you are:
- Pregnant
- Allergic to albumin (egg allergy)
Or if you suffer from:
- Myasthenia Gravis
- Lambert-Eaton Myasthenic Syndrome (LEMS)
- Amyotrophic Lateral Sclerosis
What happens after the treatment?
You should be able to eat and drink as soon as you feel up to it. Once you have passed urine you will be discharged from the hospital. You will be advised to rest on the day of treatment and return to your normal activities as you feel able. A follow up appointment will be arranged by your consultant.
Seeking further help
If you are having any difficulty in emptying your bladder or with incontinence after the Botox® treatment, please contact the Gloucestershire Bladder and Bowel Health or the Urogynaecology team for further advice.
Contact information
Gloucestershire Bladder and Bowel Health
Oakley Suite (2nd floor Centre Block), Cheltenham General Hospital, Sandford Road GL53 7AN
Tel: 0300 422 5305
Monday to Friday, 8:30am to 3:30pm,
Email: ghn-tr.gloscontinenceservice@nhs.net
Urogynaecology Department
Gynaecology Out-patients, Women’s Centre, Gloucestershire Royal Hospital, Great Western Road, Gloucester GL13NN
Tel 0300 422 6246
Monday to Friday, 8:30am to 3:30pm
Further Information
The following websites will give you more information about Botox.
The British Association of Urological Surgeons (BAUS)
www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/Botox.pdf
The British Society of Urogynaecology (BSUG)
https://bsug.org.uk/budcms/includes/kcfinder/upload/files/info-leaflets/Botox-BSUG-Dec-2019(1).pdf