Continuous Subcutaneous Insulin Infusion (CSII) pump therapy
This booklet has been written by the Insulin Pump Therapy Team to standardise the information given to patients about Continuous Subcutaneous Insulin Infusion (CSII) pump therapy in Gloucestershire. We advise that you and/or your family read this booklet and keep it in a safe place for reference when needed.
On this page
-
Information about CSII Pump Therapy
-
Clinic appointment
-
First days using an insulin pump
-
Potential causes of hypoglycaemia
-
Hypoglycaemia management
-
Potential causes of hyperglycaemia
-
Hyperglycaemia guidelines
-
Managing sick days
-
Managing Hyperglycaemia on a Hybrid Closed Loop system (HCL)
-
Converting back to insulin pen injections
-
Converting back to insulin pump therapy
-
Insulin pumps and hospitals
-
Investigations
-
Traveling by air with your insulin pump
-
Other travel information
-
Testing basal rates
-
Contact information
Information about CSII Pump Therapy
Insulin pump therapy is used by patients with type
1 diabetes who are unable to reach target blood glucose (glycated haemaglobin, or HbA1c) levels with multiple daily injections.
Insulin pump therapy only uses rapid insulin. If there is a problem with the delivery of insulin, the blood glucose level will rise rapidly.
Therefore, it is important for you to monitor your blood glucose for a minimum of 4 to 8 times through each day and night, either with finger prick blood glucose, intermittently scanned glucose monitoring (isCGM) or real time continuous glucose monitoring (rtCGM). For simplicity, we will be referring to both isCGM and rtCGM as ‘sensor glucose’ in this booklet.
Diabetes Ketoacidosis (DKA) may happen if your blood glucose level rises to 13.9mmols/L or above and is not treated.
DKA is a serious medical condition caused by very little or no insulin in the body. A lack of insulin in the body means that the glucose remains in the blood stream and cannot enter the cells to provide energy. The body responds by producing more glucose and eventually breaks down body fat to produce energy.
DKA requires urgent hospital treatment and if not treated properly it can be life threatening.
Clinic appointment
After starting insulin pump therapy, you will be sent an appointment to see the Diabetes Consultant in the Insulin Pump Clinic. This appointment will give you the opportunity to discuss if pump therapy has been successful and whether you have benefitted from using an insulin pump. If your diabetes control shows no improvement, pump therapy may be discontinued. This will be discussed with you and reviewed at each clinic visit.
During your consultation, your fasting basal charts or sensor glucose data will be reviewed.
Please upload your glucose monitoring device and/or pump prior to the clinic appointment to provide information to help optimise your glucose levels.
The following pumps, T:slim™ and Omnipod® system can be downloaded to your GLOOKO account. You can export your data from the DANA I pump to share via PDF. If you use a Medtronic 780G pump you can use the Carelink app on your phone and the information will automatically upload to the cloud, if not, please manually upload to Carelink.
You will be invited to attend the joint pump clinic with the Specialist Diabetes Nurse and Dietitian if you need further support. You will also have the opportunity to attend an insulin pump refresher group to update your knowledge on pump management.
First days using an insulin pump
During the first few days of insulin pump therapy, your blood glucose levels may be erratic and take time to settle.
This is due to a different method of delivery of basal insulin and any remaining basal insulin from your last basal injection.
The aim of pump therapy is to keep fasting blood glucose levels between 4 to 7 mmol/L. However, this depends on the individual and personal targets can be discussed with your diabetes team. If you have no hypoglycaemia awareness you may be given a different blood glucose target range.
For the first 72 hours, you should monitor your glucose levels either via finger-prick blood glucose or sensor glucose every 2 hours.
You may need to continue monitoring 2 hourly if your levels vary. Once your glucose levels are stable, we advise as a minimum that you monitor your glucose on waking, before food, at bedtime, before and after exercise and before driving.
For ongoing care, you must:
- Change your metal cannula every day.
- Change your Teflon cannula every 2 to 3 days, unless otherwise stated.
- Monitor your glucose levels 2 hours after inserting a new cannula. Try not to perform cannula changes at bedtime.
- Do not remove your old cannula until the new cannula is in place and secure.
- Change the cartridge/reservoir and tubing every 3 to 6 days (depending on the pump manufacturer instructions).
- Change your insulin Pod every 3 days and test your glucose after 1½ hours.
Always keep a supply of backup insulin pens in case of an emergency, i.e., for correction bolus by pen, or changing/reverting back to insulin injections. Check the insulin expiry dates regularly and keep a record of your daily basal insulin, basal insulin profile, insulin to carbohydrate ratio and correction ratio/insulin sensitivity in case of pump failure.
Potential causes of hypoglycaemia
- An increase in physical activity
- Drinking alcohol
- Priming a new infusion set while it is still attached to the body
- Infusing insulin through damaged sites, for example areas of lipohypertrophy (the over use of injection/cannula sites which affects the absorption of insulin)
- Basal rates are set too high
- Failure to cancel or reduce a set temporary basal rate on certain pumps
- Errors in handling the pump/PDM
- Miscalculation of a bolus
- Giving over 6 units in one bolus dose (it is recommended to split the dose or use advanced bolus options if over 6 units are needed) due to increased sensitivity to insulin. Please ask a member of the team if you would like more information about this
- Over correction of a high blood glucose
- Slow digestion of food
- Stress
- Menstrual cycle
- Incorrect carbohydrate or correction ratio
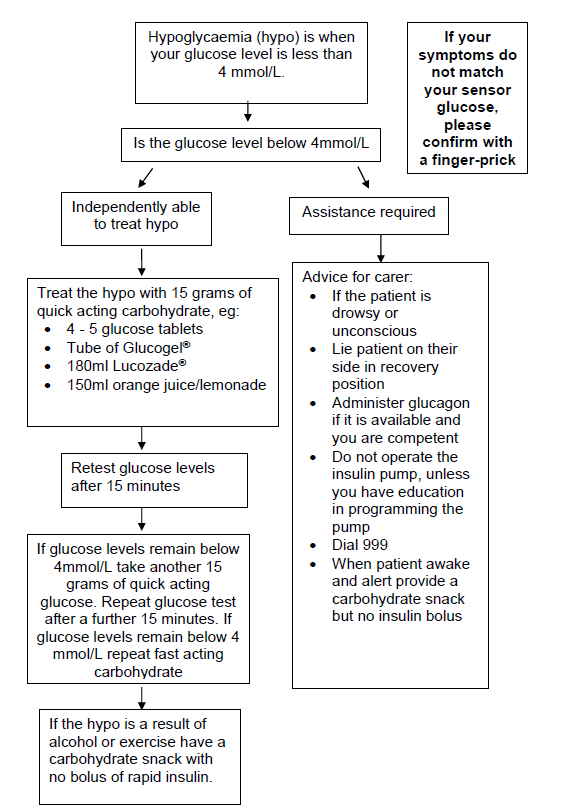
Hypoglycaemia management
Potential causes of hyperglycaemia
- Increased insulin requirements
- Illness or infection
- Reduced physical activity
- Stress
- Hormonal changes such as menstrual cycle
- Medication, such as steroids
- Inflammation at infusion site
- Insufficient insulin delivery
- Miscalculation or forgetting to administer insulin bolus dose
- Excessive amount of carbohydrates following hypoglycaemia
- Rebound from hypoglycaemia
- Basal rates set too low
- Too much time off the pump/Pod
- Pump not functioning/pump in stop mode/incorrect operation of the pump/battery is low or expired
- Insulin is not effective - for example the insulin has expired, been in use for more than a month, near the end of the vial, crystallised, cloudy or been exposed to extreme temperatures
Infusion set
- Infusion set blocked, kinked or the cannula has become dislodged
- Infusion set/Pod empty or not primed
- Infusion set leaking at the connection between the tubing and cannula
- Air or blood in the tubing
- Infusing insulin through an area of hypertrophy (tough, thickened skin)
- Empty cartridge/reservoir/Pod
- Cannula has bent or has slipped out of your skin
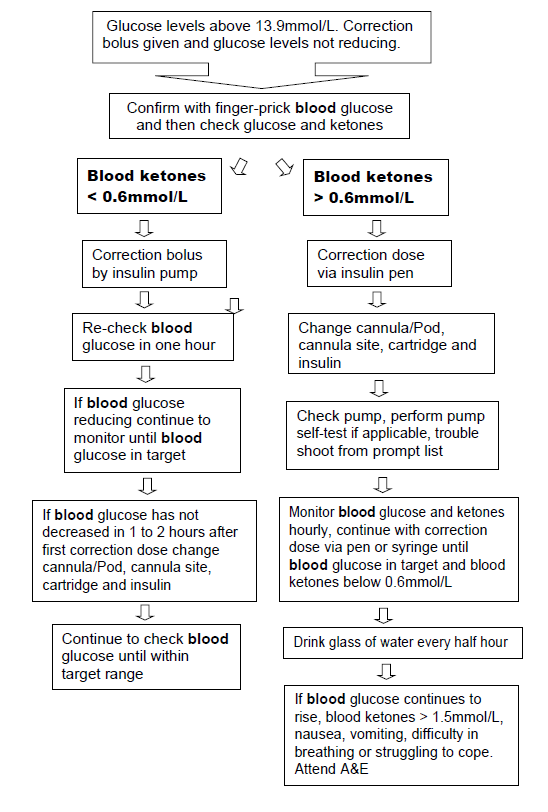
Hyperglycaemia guidelines
Managing sick days
When you are unwell there is a rise in glucose levels due to the body’s response to illness.
Glucose levels rise even though you may not be eating and drinking normally, as the body releases stored glucose from the muscles and the liver. Therefore, you may need extra insulin during this time to keep your blood glucose levels within target and prevent ketoacidosis.
Suggested temporary basal rate increases when using a pump not in hybrid closed loop:
- Minor illness such as a cold – increase the basal rate by 25% to 50%
- Severe illness or infection – increase the basal rate by 50% to 100%
- The number of hours that a temporary basal increase is required will vary. We advise you review your temporary basal at least every 12 hours
- Test your glucose levels 2 hourly while using the temporary basal rate function and confirm your sensor glucose levels with a finger-prick blood glucose
- Consider increasing the bolus dose for food by 50%
- Please refer to hyperglycaemia flow chart above
Managing Hyperglycaemia on a Hybrid Closed Loop system (HCL)
Minor Illness
- Try to stay in closed loop and change your cannula, infusion set and reservoir. The system will try and cope with raised glucose levels by increasing your basal and delivering a bolus.
- Check that your sensor glucose matches your blood glucose.
- Check to see if a manual correction is needed via the bolus calculator.
- Check glucose and ketones levels every 2 to 4 hours (please refer to hyperglycaemia guidelines on page 8).
- Drink plenty of sugar free fluids.
Exiting Hybrid Closed Loop:
- It is likely that your pump will exit closed loop if it is unable to manage your sensor glucose levels.
- This means it will revert back to manual mode and the basal rate settings that you have programmed. However, HCL pump systems vary so please check with your diabetes team if you are unsure.
- While the pump is in manual mode, please consider (in addition to the above):
- Giving a correction dose of rapid insulin via an insulin pen
- A temporary basal rate increase
- You must never stop your pump
- Re-enter closed loop when:
- Blood glucose/sensor glucose levels are stable
- Ketone levels are in normal range
- You no longer require a temporary basal rate
- It has been more than 4 hours since you gave your last correction dose via a pen.
Converting back to insulin pen injections
In certain circumstances it may be necessary for you to go back to your previous regime of 4 injections a day (basal bolus).
To make the change back to basal bolus therapy, you should take your total basal insulin dose plus 10%, or your average basal insulin use per 24 hours over the last 5 days if you are using HCL plus 10%. Be mindful that this is a starting point and if you are using pens for some time, it may need increasing further. It is advisable to take the basal insulin in the morning.
You can continue with your usual insulin to carbohydrate ratio for your fast acting insulin.
Converting back to insulin pump therapy
When restarting insulin pump therapy, there will be active basal insulin present from you last basal insulin injection, therefore you will need to test your glucose levels 2 hourly to start with.
A temporary basal reduction may be needed in the first 24 hours. If you are using a HCL system you may need to wait 48 hours before activating HCL mode. This may vary depending on the system you are using, please check with your diabetes team.
Insulin pumps and hospitals
For any hospital admission it is essential that the medical and nursing staff are aware that you are using an insulin pump.
It is therefore important that you carry some form of identification with you at all times such as a medic alert disc or a pump identification card stating that you have diabetes and are using an insulin pump.
- You may be able to continue using your pump during your hospital stay if this is agreed with the medical team.
- Remember to take with you all the necessary equipment for your insulin pump as this will not be available on a hospital ward.
- If you are unable to manage your pump independently then your diabetes will need to be managed with conventional therapy, such as subcutaneous injections or IV insulin and dextrose infusion.
- Do not remove the pump/Pod until either sliding scale insulin and intravenous fluids, or insulin administered by pen or syringe is established.
Investigations
Certain examinations can interfere with the operation of the insulin pump/Pod for example an MRI scan (Magnetic Resonance Imaging), X-ray and CT scans (Computed Tomography).
You must remove the insulin pump, Pod, transmitter and sensor if applicable and store safely outside the room. If you do not remove the pump, it may affect the warranty.
If your procedure lasts longer than 1 hour, you will need to have either sliding scale insulin commenced or a bolus dose of rapid insulin.
Traveling by air with your insulin pump
Requirements:
- Type 1 identification.
- Pump travel letter.
- A copy of your latest prescription.
- This pump booklet - we can provide you with an electronic copy if you prefer
- Contact details for your pump company, listed at the end of this booklet.
- Pump equipment and consumables. Some pump companies will be able to loan you a spare pump for your holiday. Please check with your company.
- Insulin vials for your pump.
- Back up insulin pens, needles, basal and rapid insulin.
- Blood ketone meter and strips
- Hypo treatment
- Blood glucose meter and strips
Pack your insulin and pump supplies in your hand luggage. The temperature in the luggage hold could freeze your insulin and cause it to become inactive.
Take double your insulin consumables to cover the holiday. Remember to take both your insulin for your pump AND your long acting and rapid acting insulin in pens.
You may have to store your diabetes equipment in a secure area of the aircraft depending on the flight company regulations.
Metal detectors will not harm your pump, Pod or PDM and will not normally activate security alarms. It is advisable to notify the airport security that you are wearing an insulin pump.
Insulin pumps and blood glucose meters that are active must not go through X-ray unless the batteries are removed.
If you have to have a body scan, disconnect the pump from your body; it cannot go through the body scanner unless the batteries are removed.
If your pump is operated by Bluetooth, the Bluetooth function may have to be switched off - please check with the airline before you fly.
If you use an insulin pump with a sensor, please follow the guidance from the manufacturer of the sensor with regards to travel and airport regulations.
Check the tubing and insulin cartridge for air bubbles frequently. Atmospheric pressure from altitude may affect insulin delivery from the pump and cause air bubbles. If this happens then you will need to prime the infusion line.
Omnipod® insulin pumps can be operated during the flight.
Other travel information
You may wish to return to pen therapy for your holiday. Please speak with a member of the diabetes team if this is something you would like to do.
If you are travelling to a country with high temperatures:
- You may be more susceptible to hypos, due to the increased absorption of the insulin.
- Consider making adjustments to your basal rates depending on your blood glucose levels.
- Direct exposure from the heat to the pump/Pod may affect the efficiency of the insulin and require the cartridge/Pod and tubing to be changed more frequently.
- Dehydration and hyperglycaemia can lead to ketoacidosis.
- On arrival at your destination, change the pump/PDM time to local time, your basal rates will automatically change.
- Never change the battery or insulin cartridge on the beach, sand may enter the cartridge chamber and affect the movement of the piston rod.
Testing basal rates
One of the key advantages of insulin pump therapy is the ability to tailor basal rates in ways not possible with insulin injections.
You should test your basal rates by fasting with every season change, or every 3 months and before your hospital appointment if you would find it useful.
You should test the basal rate first, during the night. Once you have the correct overnight basal rate set, you can move on to testing the basal rates in the first part of the day. Test basal rates in sections of the day rather than fasting for the whole day.
If you are using a HCL system you may not need to test your basal rates as the insulin pump will adjust these for you, based on its algorithm. However, it is important that you regularly review your basal rate settings within the manual mode on your pump. This is to make sure that you are on the correct amount of insulin if you need to revert to manual mode.
You can do this by regularly reviewing your total basal rate in the closed loop and comparing it with the total basal rate you have saved in your manual settings. Please ask your DSN/dietitian if you would like support adjusting this.
Remember, optimising your basal rates is key to optimising your pump.
- Aim is to keep all glucose levels 4 to 7 or 5 to 8 mmol/L.
- Test your glucose levels 2 hourly during a fast. This can be either sensor glucose or finger-prick blood glucose levels.
- Choose a time when your blood glucose is within target before testing fasting basal rates, but not at the expense of a correction dose. Should you need to give a correction dose, check your blood glucose after 1 hour, if it is within target start fasting.
- Try not to eat a meal high in fat before fasting as this will have an extended effect on your blood glucose.
- No alcohol should be consumed in the previous 24 hours.
- Avoid if you are premenstrual.
- If your basal rates need changing, increase or decrease the basal rate 2 hours before the out of target blood glucose by 0.1
Once you have your basal rates correct, then you need to check if your carbohydrate ratio is correct. Test your glucose levels before and 2 hours after your meal. If your glucose rise is more than 2.8 mmol 2 hours after your meal, you should consider reducing your carbohydrate ratio with that meal so that it offers you more insulin.
We recommend that you always keep a record of your current pump settings, carbohydrate ratios and insulin sensitivity ratios, so that in the event of a pump failure or the unexpected requirement for a new pump you can use these settings.
Contact information
The Diabetes Pump Therapy Team
Gloucestershire Royal Hospital
Tel: 0300 422 8613
Monday to Friday, 9:00am to 4:00pm
Cheltenham General Hospital
Tel: 0300 422 4266
Monday to Friday, 9:00am to 4:00pm
E-mail: ghn-tr.diet.diabetes@nhs.net
E-mail: ghn-tr.diabetesnurses@nhs.net
For technical advice, please call the pump company helpline:
Medtronic
Tel: 01923 205 167
Insulet (Omnipod)
Tel: 0800 011 6132
Air Liquide (Tandem T-Slim)
Tel: 08000121560
Advanced Therapeutics
Orders and technical queries
Tel: 01926 833 273
Monday to Sunday, 9:30am to 5:30pm
Technical support emergencies
Tel: 07775 642239