Having a diagnostic gastroscopy as an outpatient
You have been advised to have a gastroscopy, which you may also have heard being called an endoscopy or OGD (meaning an oesophageal-gastro-duodenoscopy). A diagnostic gastroscopy will help us to investigate the cause of your symptoms.
It is important that you read this page before your appointment so that you understand what will happen during this procedure and the preparation involved.
If you have diabetes and you are receiving treatment, please leave a message on the Medication Advice Line; a member of the team will return your call. The telephone number is at the end of this page.
If you are using an insulin pump, we would like your BM to be 7mmol/L. Please call your local pump team if you need further advice.
If you are taking any medication that thins your blood, other than aspirin (which you can continue to take), please contact the Medication Advice Line.
This is very important as your procedure may be delayed if you do not get advice.
If required, you may be asked to attend the radiology department for imaging tests on the same day as your gastroscopy.
What is a gastroscopy?
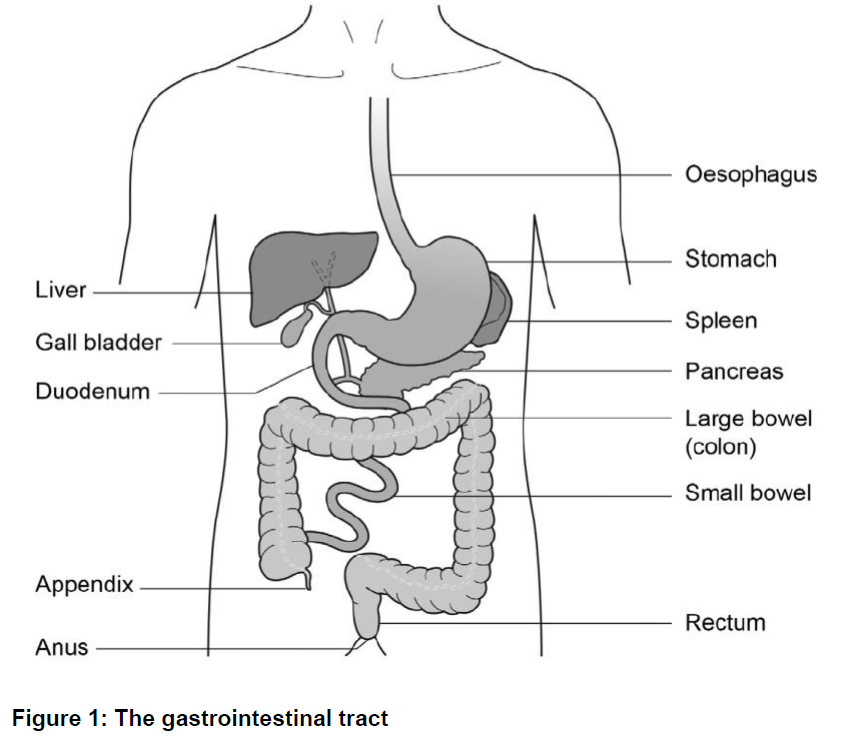
Gastroscopy is an investigation to look directly at the lining of the oesophagus (gullet/food tube), the stomach and around the first bend of the small intestine (the duodenum). A gastroscope is passed through the mouth, down the oesophagus and into the stomach.
A gastroscope is a long flexible tube, thinner than your little finger. It has a bright light at the end (this is not hot), which is necessary to be able to see the lining of the stomach. Pictures are transmitted on to a screen where any abnormalities can be seen.
If required, a biopsy will be taken. A biopsy is a small sample of tissue that may be taken from the lining of your gut or bowel for further examination in the laboratory. It is taken using sterile biopsy forceps through the scope. This will not be painful.
Alternative procedures
The main alternative to a gastroscopy is a barium meal X-ray.
This can look at the stomach, but does not allow biopsies to be taken. Please note that an alternative procedure will not be available on the day.
Preparing for your procedure
To allow a clear view during the procedure the stomach must be completely empty. You are therefore asked not to have anything to eat for at least 6 hours before your appointment time.
You may sip water up to 2 hours before your appointment time.
The NHS, a major contributor of carbon emissions in the UK, has recently outlined ambitious targets to achieve net zero carbon emissions by 2040. The endoscopy team in Gloucestershire have carefully considered ways of adopting more sustainable care and waste reduction.
We would appreciate your support to help make our practice ‘greener’ by kindly bringing the following items along to your endoscopy appointment, so that single use alternatives are not required:
- If applicable, your own denture pot, hearing aid case(s) and/or eye glasses case
- Water bottle
- Reusable cup with lid for a complimentary hot drink after the procedure
- Bag to place your clothes in during procedure
On admission
On arrival at the department, you will be seen by a nurse who will check your personal details.
You will be asked a series of questions about any operations or illness that you may have had or are presently suffering with.
Please bring a list of all medications you are currently taking.
The nurse will also ask if you have any allergies or have had any reactions to medicines or foods in the past.
You might also be given a small dose of Infacol®, by mouth, to reduce the secretions in your oesophagus and bowel. Infacol® will also help give a better view of your oesophagus and stomach during the procedure. Please do not have any other liquids after you have been given the Infacol® - the nurse giving you this medication will also remind you not to have any further fluids.
You will be offered a choice of throat spay and/or sedation. If you are considering sedation, you will be asked to confirm that you have a responsible adult to escort you home when you are ready for discharge.
You must also have a responsible adult with you at home for 24 hours following the procedure.
The test and possible complications will be explained so that you understand the procedure and any risks involved.
You will be asked to sign a consent form. By signing this form, you will have agreed to have the test performed and that you understand why it is needed. This does not take away your right to have the test stopped at any time.
For the time that you are in the department we want to provide a safe, supportive and pleasant environment. Please do not be afraid to ask if you have any worries or questions at this stage.
For this procedure you will not need to remove your clothes but ties may need to be loosened and shirts opened if they are tight at the neck.
Please remember that your appointment time is not the time you will have your procedure. There will be a wait between your admission and having your test done.
A nurse or doctor will escort you into the room where your procedure will take place. A nurse will stay with you throughout the test.
The Endoscopy Units at Cheltenham General and Gloucestershire Royal Hospitals are training centres. This means that there may be Registrars and Nurse Endoscopists performing the procedure under the supervision of an experienced endoscopist.
Students may also be observing the procedures. Please let the admitting nurse know if you have any concerns about this.
Sedation or throat spray
Intravenous sedation and/or local anaesthetic throat spray can improve your comfort during the procedure. Intravenous sedation will make you lightly drowsy and relaxed, but not unconscious (asleep).
Anaesthetic throat spray
Throat spray is a local anaesthetic spray used to numb the throat. This can be given on its own or alongside sedation.
As the gastroscopes have become thinner, many patients are happy for the procedure to be carried out without sedation and to have throat spray only.
The throat spray has an effect very much like a dental injection.
The benefit of choosing throat spray is that you are fully conscious (awake) and aware during the procedure and you will be able to go home unaccompanied.
You will not be allowed to have anything to eat or drink for about 30 minutes after the procedure. This will allow time for the sensation in your mouth and throat to return to normal.
It is strongly advised that your first drink after the procedure should be cold. This will be given before you are discharged and should be sipped slowly to make sure that you do not choke.
After discharge you will be able to carry on with your normal routine.
Intravenous sedation
Sedation will be given though a cannula (thin tube) inserted into a vein in your hand or arm. This will make you feel lightly drowsy and relaxed but not unconscious (asleep). You will be in a state called conscious sedation. This means that, although drowsy, you will still hear what is said to you and therefore will be able to follow simple instructions during the procedure. You will be able to breathe normally throughout the procedure.
While you are sedated, we will check your breathing and heart rate so changes will be noted and dealt with accordingly. For this reason, you will be connected by a finger probe to a pulse oximeter which measures your oxygen levels and heart rate during the procedure. Your blood pressure will also be recorded.
Oxygen will be given to you via a mask or a small sponge inserted into your nostril.
Please note that if you decide to have sedation you are not allowed to drive, drink alcohol, operate heavy machinery or sign any legally binding documents for 24 hours following the procedure. You will need someone to accompany you home and a responsible adult to stay with you for 24 hours.
The procedure
In the examination room any dentures will be removed and a local anaesthetic spray will be applied to the back of your throat to numb it for the procedure.
Once you are in a comfortable position on the trolley, a plastic mouth piece will be put between your teeth or gums, if dentures have been removed. This helps to protect your teeth and the gastroscope.
If you have chosen to have sedation this will be given into a vein through a cannula in your hand or arm. The sedation will be allowed to work for a couple of minutes and then the procedure will commence.
The tube will then be inserted through the mouth piece. When it reaches the back of the throat you may be asked to swallow to help the tube go down into the stomach. This will not interfere with your breathing.
Some air will be passed through the instrument to inflate your stomach to allow a clearer view. You may feel wind like discomfort and belch some air up during the test. Please do not be embarrassed.
Any saliva in your mouth will be removed using a small suction tube. When the gastroscope is taken out, most of the remaining air in the stomach will also be removed.
The gastroscopy normally takes between 5 and 15 minutes.
Possible complications
Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems occur, they are normally short lived. Careful monitoring by a fully trained endoscopy nurse makes sure that any potential problems can be identified and treated rapidly. Older patients and those who have health problems, for example, people with breathing difficulties due to a bad chest, may be assessed by a doctor before being treated.
Minor complications with sedation happen in less than
1 in every 200 examinations. A few people are excessively sensitive to the sedation we use and become too sleepy. This effect can be rapidly reversed with another injection.
Major complications with endoscopies are very rare (less than 3 in every 10,000) and death arising from these is extremely rare (less than 1 in every 30,000).
The main serious complication is perforation (a tear) of the oesophagus (gullet) or bowel, which may need an operation and stay in hospital.
After the procedure
After the gastroscopy is completed, the nurse caring for you during your test will take you from the endoscopy room to the recovery area.
Your pulse and blood pressure will be monitored as needed. This is called the recovery period. You may feel a little bloated or have some discomfort in your lower abdomen after the test. You will need to stay in hospital for about an hour after the procedure depending on how you recover from the sedation.
If sedation has not been given, you will be allowed home once the throat spray has worn off and you have had a drink.
Normally you do not see the person who performed your procedure before going home.
Your nurse will tell you the results of the test before you are discharged. If you have had sedation, it is a good idea to have someone with you at this discussion as many people find they forget what has been said to them.
If a sample (biopsy) has been taken, the result can take up to 5 weeks to process. You may be given an outpatient’s appointment to return for review. Alternatively, the results will be forwarded to your GP; you will need to make an appointment to discuss the results.
Please contact your GP or consultant directly for your test results as these are not disclosed to Endoscopy.
A report of the procedure will automatically be sent to your GP.
Going home
If you have had sedation, it is essential that someone takes you home and that there is a responsible adult to stay with you for 24 hours.
Important note:
Important note: You may go home by taxi but you must have someone to accompany you on the journey.
For this period of time, you should not:
- Drive a car, motorbike or ride a bicycle
- Drink alcohol
- Operate machinery or do anything requiring skill or judgement
- Make important decisions or sign any documents
If sedation has not been given the above paragraph does not apply.
You will be given a discharge advice leaflet before you leave the unit.
Contact information
Appointment Enquiries (answerphone)
Tel: 0300 422 6350
Tel: 0300 422 6351
Monday to Sunday, 8:30am to 4:00pm
Medication Advice Line (answerphone)
If you have any questions relating to your medication, please ring the number below for the hospital you will be attending and leave a message. A member of staff will return your call, normally within 24 hours, week days only.
Cheltenham General Hospital
Tel: 0300 422 3370
Monday to Friday, 8:00am to 6:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 8232
Monday to Friday, 8:00am to 6:00pm
Saturday to Sunday, 9:00 to 12:00 Midday
Other Endoscopy Units
Cirencester Hospital
Tel: 0300 421 6294
Monday to Friday, 8:00am to 6:00pm
Stroud General Hospital
Tel: 0300 421 8073
Monday to Friday, 8:00am to 6:00pm