Improving bowel function and control
This page gives you hints and tips to help improve your bowel function and control. Also included is information about bowel routine, skin care and dietary advice.
On this page
-
Bowel function
-
Regular bowel routine
-
Exercise
-
The correct position for opening your bowels
-
Self-abdominal massage
-
How to perform abdominal massage
-
Anal sphincter exercise
-
The Bristol Stool Chart (BSS)
-
Advice for diarrhoea, bowel frequency and urgency
-
Controlling wind and smells
-
Drinking
-
Disguising smells
-
Skin care for people with bowel problems
-
Tips to prevent skin soreness
-
If your skin is already sore
-
Dietary fibre advice
-
How much fibre should I eat?
-
How can fibre help with bowel control?
-
Increasing your dietary fibre
-
Examples of dietary fibre content
-
Contact information
-
Further information
Bowel function
Poor bowel function and/or loss of bowel control may be an upsetting and embarrassing problem that can affect your everyday life. There are many different causes of this problem, some of which are listed below:
- Constipation made worse by ill health, poor diet and dehydration from lack of fluid.
- Some medications such as antidepressants, pain relief and iron tablets.
- Bowel diseases (such as Crohn's Disease, IBS, diverticulitis).
- Neurological disease (such as Multiple Sclerosis, Stroke, Parkinson’s disease).
- Diarrhoea.
- Damage or weakness of the muscles around the anus, resulting in the muscles not being able to hold back the stools until you are able to get to the toilet.
Your doctor or nurse will try and find the cause of your problem so that the best treatment can be planned for you. While you are waiting for your treatment plan, this page will give you information about the symptoms you are experiencing and tips about how to manage them better.
Regular bowel routine
A regular bowel routine will help to ease your symptoms. Usually, the bowel is most active after a meal but warm drinks such as tea or coffee can also trigger bowel activity.
Make good use of this increased bowel activity by trying to have your bowels open when your bowel is most active 15 to 20 minutes after food or drink (such as after breakfast or lunch). Set aside this time of the day for your bowel movement.
Exercise
Exercise stimulates the bowel to work, leading to easier bowel emptying. Exercise does not have to be rigorous. Simple day to day exercise gained from daily living (such as walking or housework) will help.
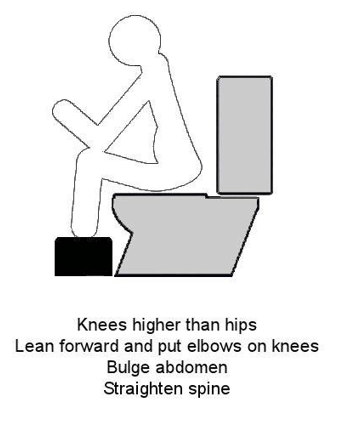
The correct position for opening your bowels
Sitting in the correct position on the toilet will make it easier for you to empty your bowels. Follow the steps below to get into the most effective position.
Step 1
Sit on the toilet and raise your feet onto a foot rest (a stool or even a pile of books will do). The aim is for your knees to be higher than your hips.
Step 2
Lean forwards, with a straight spine and rest your elbows on your knees.
Step 3
Bulge out your abdomen and pretend you are gently blowing out candles on a birthday cake. Rest and then do this again. Do not sit on the toilet for longer than 10 to 15 minutes and do not strain. You should be able to empty the bowel with very little effort.
If your stool is very hard it can be even more difficult to pass and can feel as if it has gotten stuck. The following technique can help:
- Hold something soft in your left hand such as a stress ball.
- Rest it on your tummy, on the left side and put your right hand over the top.
- Rock yourself forward and rest, then rock yourself back and push out the stool.
- Try this for 5 to 10 minutes.
Remember: Make sure the toilet seat is comfortable (not too cold) and allow yourself enough time and privacy.
Self-abdominal massage
What is it for?
Abdominal massage has been used as a treatment for constipation for many years and can:
- promote contractions of the large intestine which moves faecal matter along the gut.
- speed up the time it takes stool to move through the intestines to the anus.
- soften stool and make it easier to pass.
- relieve abdominal pain caused by cramps/wind.
- reduce the need for laxatives.
People like the fact that abdominal massage does not involve medications. They can do it themselves and there are no side effects.
How to perform abdominal massage
Abdominal massage works best when you make it part of your bowel routine. It will take about 10 minutes.
To perform abdominal massage, you should:
- Lie down on your back with a pillow under your knees, for example, on your bed with pillows under your head and knees. Feel free to adapt this position as you need to be comfortable.
- Start in the small of your back with both hands, move your hands forwards over your hips and down both sides of the pelvis towards your groin. Repeat this about 10 times.Now start the massage on the right side near the pelvic or hip bone and apply pressure in a circular motion, working the hands up to the rib cage. Continue for about 2 minutes if this feels comfortable.
- Move your hands to the left side, continue working them down to the pelvic or hip bone, then come back up towards the belly button increasing pressure in a clockwise direction around the presumed course of the large intestine. Imagine you are trying to squeeze toothpaste out of a tube. Repeat from top to bottom about 10 to 15 times. Spend 2 minutes kneading downwards, then 2 minutes kneading up the right side and lastly spend 2 more minutes kneading down the colon.
- Finally stroke gently across your tummy 10 times to help your body know the massage is ending.
Please copy the following link into your web browser to watch a video of a carer massage and a self-massage:
www.youtube.com/watch?v=gbQo49QsTO8
Remember, it can take 6 to 8 weeks before the abdominal massage starts to help.
Anal sphincter exercise
Anal sphincter (the ring of muscle around your back passage) exercises can help you to improve your bowel control. When done correctly these exercises can build up and strengthen the muscles to help you to hold both wind (gas) and stool in the rectum (back passage).
Your doctor or nurse will be able to teach you how to do the exercises and will give you a leaflet with the same information, to help you remember at home.
To get the best results, you must practice the anal sphincter exercises every day for 3 to 6 months.
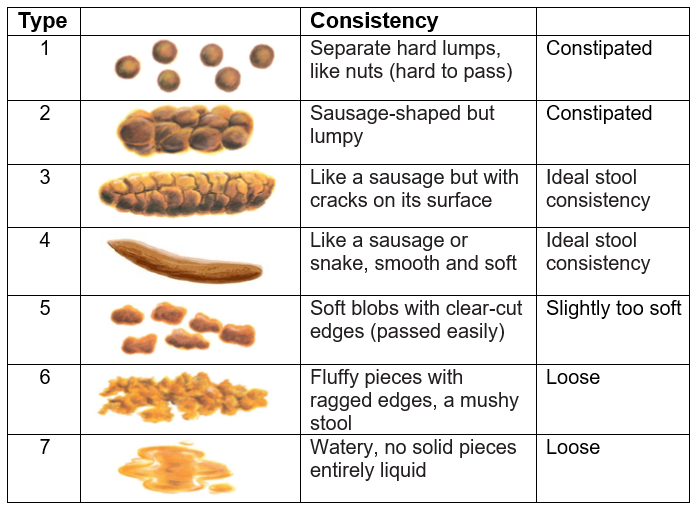
The Bristol Stool Chart (BSS)
This is a tool that helps you identify what type of stool you are passing and is useful information for your health care practitioner.
Knowing what type of stool you are passing is important to understand your bowel health. A type 3 or 4 stool is the ideal stool to pass.
Advice for diarrhoea, bowel frequency and urgency
If you have diarrhoea or bowel urgency (having the sudden feeling of wanting to have your bowels opened), you may find the following advice helpful:
- Limit caffeine and high fat foods as these stimulate the bowel and can cause it to contract or spasm, which may cause bowel urgency.
- Avoid foods that contain sorbitol (an artificial sweetener often used in sugar free sweets and chewing gum) as these can cause diarrhoea.
- Avoid antacids that contain magnesium such as Gaviscon®, as these can also cause diarrhoea.
- Removing the skins, seeds and membranes (pith) from fruit and vegetables may make them easier to digest. Canned or well-cooked fruit and vegetables may also be easier to tolerate.
- Avoid large volumes of pure fruit juice and keep portions of fruit small and spread out through the day.
- Try eating small meals more frequently throughout the day (little and often), rather than 3 larger meals.
- For some people, large amounts of milk and yogurts may contribute to loose stools. Cut down on these for 2 to 4 weeks to see if this helps. Lactose-free dairy or dairy alternatives may be tolerated better. If you think milk may be a problem, talk to your dietitian or doctor.
For some bowel symptoms, you may need to eat less fibre in your diet until the diarrhoea has stopped, then slowly go back to your normal diet.
Controlling wind and smells
When you have a bowel problem, you may find that you cannot always control wind (gas) from your back passage and that any wind you do pass smells bad.
Some foods create more gas than others, especially foods high in fibre (particularly soluble fibre) - see the dietary fibre section.
The effect of certain foods is very individual, so what causes wind for one person may not cause wind for another. It is worth trying to see if certain foods make things worse for you and whether limiting these foods will help.
Below is a list of some of the foods that commonly cause wind:
- Any type of beans (including baked beans and kidney beans)
- Peas, lentils and other pulses
- Muesli
- Bran cereal or other high bran foods
- Brown rice or wholemeal pasta
- Nuts (especially peanuts)
- Cabbage, cauliflower, sprouts and artichoke
- Eggs
- Shellfish
- Milk and milk products
- Salad (especially cucumber & lettuce)
- Apples, watermelon, dried fruit
- Onion, garlic and leeks
- Slimming foods and sugar free products containing added fructose or products containing sorbitol/ mannitol such as chewing gum
- Hot spicy foods
- Rich, fatty foods
Sometimes the way in which you eat means that you swallow a lot of air with your food. Try eating a little more slowly. Chew each mouthful carefully (especially if the food is high in fibre) and take care not to talk too much while you are eating. Even if you are in a hurry, do not be tempted to rush your food or wash down half chewed food with a gulp from a drink.
Eating little and often, rather than one huge meal a day, can make it easier for your intestines to digest and as a result, produce less gas. Regular meal times can also help as an empty stomach can produce more wind and gurgles.
Drinking
Caffeine in tea, coffee and cola has a tendency to stimulate bowel activity for some people. It can increase wind and give some people urgency to pass a stool. Drink decaffeinated tea and/or coffee for a week or two, to see if this makes any difference.
Fizzy carbonated drinks, beer and lager can increase wind production for some people. Often you will burp but some people can experience more wind with these drinks. Excess alcohol can cause more wind than usual the next day.
Sometimes doing anal sphincter exercises to strengthen the muscles can improve your control of wind (see the Anal sphincter exercises section).
Disguising smells
If you produce a lot of wind that you cannot control, some of the ideas below might help:
- Make sure there is good ventilation in the room you are in.
- Use aerosol air fresheners with care. Some smell very obvious, or even worse than the smell you are trying to disguise.
- There are many solid block air fresheners that work all of the time (available from chemists and supermarkets).
- Sprinkling a few drops of essential oils into the room, such as lavender or lemon oil, may be useful.
- Try striking a match and then blowing it out immediately and allowing the plume of smoke to drift into the room.
Peppermint oil capsules, charcoal tablets, aloe vera capsules or drinks, cranberry juice and pre and pro biotic drinks such as Yalkult® have been found to be helpful for some people in reducing wind or the smell from wind.
Skin care for people with bowel problems
Anyone who has frequent bowel motions, diarrhoea or accidental leakage may, from time to time, get sore skin around their back passage. Taking good care of the skin around the back passage can help to prevent this problem.
There are several reasons why your skin may become sore. The scientific reason for itching is that it is due to chemicals in the bacteria of the stool.
- Your bowel contains digestive juices and acid, which break down your food so your body can use the nutrients in it. If you have liquid bowel motions, the diarrhoea will still contain these juices and acid, which can cause skin soreness and redness.
- If you have faecal incontinence, the small quantity of juices and acid contained in even a normal stool can damage the skin.
- If you open your bowels frequently, repeated wiping can cause damage to sensitive skin around your anus.
- With some bowel conditions, it is very difficult to wipe your bottom well enough so a small amount of faeces always seems to get left. This stool can start to make your skin sore.
- Sometimes, the area around the anus can become infected.
- If you have incontinence of the bladder and bowel, you will be more likely to get sore as the urine and faeces react together.
- People who are not eating a healthy balanced diet, are not drinking enough or not taking much exercise, are more prone to skin soreness.
- People who are generally unwell and are immobile are at increased risk of skin soreness.
Tips to prevent skin soreness
With careful personal hygiene, it is often possible to prevent skin soreness, even if you have a bowel problem.
You should:
- Wipe gently with soft toilet paper or you could try using moist toilet paper. Throw away each piece of toilet paper after one wipe so that you do not re-contaminate the area.
- Wash around the anus after a bowel action. A bidet is ideal. If this is not possible, you may be able to use a shower attachment to wash your bottom while leaning over the edge of the bath.
- Use a soft disposable cloth with warm water. Avoid flannels and sponges as they can be rough and are difficult to keep clean.
- Specialised washes/mousses may be helpful, ask your continence nurse for advice.
- Be very gentle when drying the area. Pat gently with plain non-coloured toilet paper or a soft towel. Do not rub.
- Wear cotton underwear and change daily, to allow the skin to breathe.
- Avoid tight clothing that may rub and irritate the area.
- For women it is usually best to avoid wearing tights.
- Consider using a non-biological washing powder for underwear and towels.
- Your doctor or nurse may suggest using a barrier wipe, these are available on prescription. The barrier wipes form a protective film over the skin to protect it, especially if you have diarrhoea and are opening your bowels very frequently.
You should avoid the following:
- Do not be tempted to use disinfectants or antiseptics in your washing water as these can sting and many people are sensitive to the chemicals used in them.
- Avoid using strongly perfumed products on your bottom, such as scented soap, talcum powder, baby wipes or deodorants. Choose a non-scented soap, such as baby soap. Your continence nurse will be able to advise you.
- Avoid using any creams or lotions on the area, unless advised to do so. A few people who are prone to sore skin do find that regular use of a cream can help to prevent this. If you do use a barrier cream, wash the area regularly before applying and choose a plain type and use sparingly.
- If you need to wear a pad because of incontinence, try to make sure that no plastic comes into contact with your skin and that you use a pad with a soft surface. The continence nurse can advise you on which pads are best.
If your skin is already sore
Follow the advice you have been given about prevention. In addition, you may find that using damp cotton wool is most comfortable for wiping.
How to manage soreness/irritation around the anus:
- Use a barrier cream or ointment, as recommended by your doctor or nurse. These are available from your pharmacist. If you choose your own, try Sudocrem®.
- Try not to scratch the anal area, however much you are tempted, as this will make things worse. If you find that you are scratching the area in your sleep, you could consider wearing cotton gloves in bed (available from your pharmacist). You should also keep your nails short.
- Try to allow air to get to the anal area for at least part of every day.
Do not struggle on alone. Talk to your nurse or GP, especially if your skin is broken. If your skin always seems to be sore, you may have an infection which needs treating. There are products which can be prescribed to help heal the skin and help relieve the soreness.
Dietary fibre advice
Fibre is made up of the indigestible parts of plants, which pass fairly unchanged through your stomach and intestines. There are 2 types of fibre, soluble and insoluble.
Fibre is an extremely important part of a balanced, healthy diet. Its main role is to keep your digestive system healthy but it does have other functions within the body including:
- Controlling blood sugar levels
- Bringing down cholesterol levels
- Improving how your body uses nutrients
- Controlling your appetite
- Preventing bowel disease (IBS, diverticulitis and bowel cancer)
Soluble fibre
Soluble fibre is dissolvable in water, causing the stool to be softer, more bulky and thicker in consistency. It does this by absorbing water in the gut to produce a gel like substance which increases the size of the stool as well as softening it. Foods that contain soluble fibre include:
- Oats, barley, and rye
- Peeled fruit, root vegetables such as carrots and potatoes
- Beans and pulses
- Ground linseed or ground flaxseed
Insoluble fibre
Insoluble fibre does not absorb or dissolve in water but it holds water very effectively like a sponge, increasing stool weight. This increase in stool weight improves the movement of nutrients and waste products through the digestive tract. Foods that contain insoluble fibre include:
- Whole grains (wholemeal bread)
- Wheat and bran (cereal)
- Corn (maize)
- Nuts and seeds (except golden linseed)
- Skins of fruit and veg such as potato, apple and pear
How much fibre should I eat?
It is recommended that you should include 30g of fibre a day in your diet. This can be taken from a mixture of foods. You should also drink 8 glasses of water each day.
- A sudden increase in fibre in your diet can have 'explosive' effects and may cause abdominal pain, increased wind and bowel urgency. If you need to increase the fibre in your diet you should do this slowly, taking one extra portion of fibre containing foods every few days.
- Be aware that too much fibre in your diet can make it harder for your body to absorb certain minerals such as zinc, calcium and iron. It is best to avoid eating more than 35g of fibre per day.
How can fibre help with bowel control?
Fibre can improve stool consistency and bowel regularity, while also controlling symptoms of stool frequency and urgency.
If you tend to suffer from constipation or diarrhoea, changing the amount and type of fibre in your diet may help.
If your stools are too hard and infrequent, the aim should be to soften them to produce a stool that is easier to pass. Increasing the amount of insoluble fibre (which increases the absorption of fluid in the stool) in your diet will help to make the stool softer and bulkier.
On the other hand, if you suffer from diarrhoea or bowel urgency, reducing the amount of fibre in your diet might help. Experimenting with the fibre in your diet will help you to see which foods make your bowel control better or worse. This is very individual. Our bodies do not all react in the same way, and it is a case of trial and error to see which foods, if any, cause problems for you.
Increasing your dietary fibre
- Gradually increase your intake of fibre over a 3 to 5 day period. Make sure you also increase your fluid intake to 6 to 8 glasses per day.
- Stocking your cupboards with high fibre carbohydrate foods, such as, wholegrains cereals, oats, brown rice, rye and whole wheat crackers and breads will make it easier to include fibre in your diet.
- Always have breakfast. A regular eating pattern through the day will help your bowel to work effectively. Start the day with muesli or a high fibre cereal and try to include wholemeal or wholegrain breads as part of your breakfast routine.
- Add nuts and/or dried fruit to breakfast cereals.
- Oats contain both soluble and insoluble fibre. They are cheap, easy to prepare and delicious. Try them with freshly sliced banana and maple syrup.
- Vegetables – include plenty of vegetables with your meals, either as a side dish or added to sauces, stews or curries. Keeping a handy supply of frozen vegetables in your freezer will make sure you are never without and can be added quicky to meals.
- Eat more beans! When making casseroles, stews, curries or soups, try adding lentils, pearl barley, brown rice or cracked wheat, all of which are good sources of fibre and add flavour to any dish.
- Finish a meal with a piece of fruit, or include this as part of your mid-morning snack or lunch.
- Keep skins on fruit, potatoes and vegetables when possible.
- Choose wholegrain bread and try to cut down on your use of white bread. Choose breads that contain wholegrain kernels or contain seeds.
- Add seeds. All kind of seeds are high in fibre (sunflower, sesame, pumpkin, chia and linseed/flaxseed). Start with a teaspoon per day increasing to 1 to 2 tablespoons. Add them to soups, cereals or sprinkle over yogurt. Make sure that the flaxseed/linseed is crushed (not whole) as this is more effective in making a more fibrous stool.
- Drink more fluids. Fibre needs fluid to work in the bowel. It is really important to increase your fluid intake to make the most of the fibre you are eating. The average adult should drink 8 mugs/glasses of alcohol-free fluid per day.
Remember, the way the body reacts to dietary fibre is very individual. It may take some time for changes to fibre intake to have an effect on your bowel, and for you to find a diet you can stick to that is good for the function of your bowel. The following tables will help you decide which foods to include.
Examples of dietary fibre content
| Food Type | Portion size | Fibre content |
| Breakfast cereals | ||
| Cornflakes® | 30g | 0.3g |
| Weetabix® | 2 biscuits (37.5g) | 3.6g |
| All Bran® | 40g | 10g |
| Muesli | 40g | 3g |
| Ready Brek® (made with milk?) | 160g | 2.2g |
| Porridge | 160g | 1.3g |
| Bran Flakes | 30g | 5.2g |
| Fruit & Fibre | 40g | 2.8g |
| Sultana Bran | 40g | 4g |
| Special K® | 30g | 0.5g |
| Shredded Wheat® | 2 biscuits | 6.1g |
| Bread | ||
| White bread | 2 slices | 1.5g |
| Brown bread | 2 slices | 2.8g |
| Wholemeal bread | 2 slices | 4.5g |
| Pitta bread | 1 piece | 1g |
| Granary bread | 2 slices | 2.6g |
| Wholemeal crackers | 3 | 1g |
| Ryvita® | 2 | 2.4g |
| Pasta and rice | Cooked weights | |
| Plain pasta | 200g | 3.8g |
| Whole wheat/brown pasta | 220g | 8g |
| Boiled white rice | 200g | 0.2g |
| Brown rice | 180g | 1.4g |
| Nuts | Portion size | |
| Coconut | 25g | 1.8g |
| Peanuts | 25g | 1.6g |
| Brazil nuts | 25g | 1.1g |
| Almonds | 25g | 1.9g |
|
Food type |
Portion size |
Fibre content |
|
Fruit (80g) recommended serving |
||
| Apple (with peel) | 1 (100g) | 1.8g |
| Dried apricots | 5 pieces | 3.4g |
| Banana | 1 (100g) | 1.1g |
| Grapes | 100g | 0.7g |
| Nectarine | 1 (150g) | 1.7g |
| Peach | 1 (110g) | 1.4g |
| Orange | 1 (160g) | 2.7g |
| Pear | 1 (150g) | 3g |
| Prunes | 3 pieces | 1.7g |
| Sultanas | 1 tablespoon | 0.6g |
| Dried dates | 15g | 0.6g |
|
Cooked Fruit |
||
| Blackcurrants | 140g | 3.9g |
| Gooseberries | 140g | 2.7g |
| Plums | 140g | 1.7g |
| Rhubarb | 140g | 1.7g |
| Avocado |
½ small avocado |
3.4g |
| Vegetables | ||
| Jacket potato (with skin) | 180g | 4.9g |
| New potatoes | 175g | 2.6g |
| French beans | 90g | 3.7g |
| Cauliflower | 90g | 1.4g |
| Broccoli | 85g | 2g |
| Carrots | 80g | 2g |
| Spinach | 90g | 1.9g |
| Tomatoes | 85g | 0.85g |
| Sweetcorn | 85g | 1.2g |
| Brussel sprouts | 90g | 2.4g |
| Peas | 70g | 3.6g |
| Pulses | ||
| Split peas | 30g | 2.8g |
| Baked beans | 30g | 5g |
| Butter beans | 30g | 2.8g |
| Chickpeas | 30g | 3.4g |
| Boiled beans | 30g | 4g |
Contact information
If you have any questions or need advice, please contact the Gloucestershire Bladder & Bowel Health team and ask to speak to a Continence Specialist.
Bladder & Bowel Health (Adult)
Oakley 2nd Floor, Centre Block, Cheltenham General Hospital, Sandford Road, Cheltenham GL53 7AN
Tel 0300 422 5305
Further information
For more information about getting fibre into your diet, please visit the following websites.
NHS – How to get more fibre into your diet
Website:
www.nhs.uk/live-well/eat-well/digestive-health/how-to-get-more-fibre-into-your-diet/
British Dietetic Association (BDA)
Website: www.bda.uk.com/resourceLibrary/printPdf/?resource=fibre