Metatarsal osteotomy for a painful bunion
Following your consultation with a member of the Foot and Ankle team you have been diagnosed as needing a metatarsal osteotomy. This page gives you information about your condition and the treatment. The page will also give you some details about the recovery from surgery and common risks and complications. Please ask your surgeon if you have any further questions.
On this page
-
What is a metatarsal osteotomy?
-
Why is this type of surgery done?
-
What does the operation involve?
-
Is this a day case operation?
-
Will I have a general anaesthetic?
-
Will I have a plaster cast on afterwards?
-
Going home
-
Follow up appointment
-
Planning for your operation
-
Further advice
-
Risks
-
Contact information
-
Further information
What is a metatarsal osteotomy?
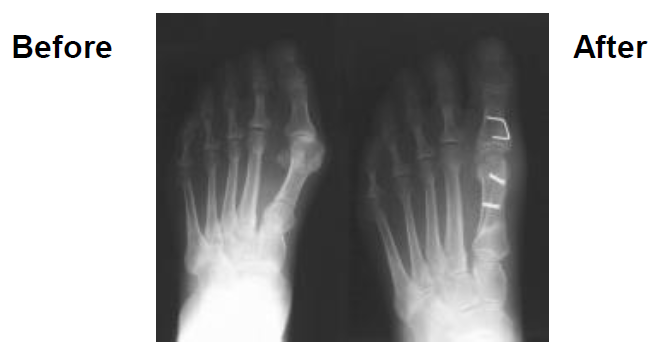
A metatarsal osteotomy is an operation for a painful bunion. The exact type of osteotomy can vary and can be known as a ‘scarf’ osteotomy or ‘chevron’ osteotomy but the operations are similar.
Why is this type of surgery done?
Sometimes, the big toe can become angled inwards, towards the middle of the foot and the second toe. This can force the top of the first metatarsal (bone) to protrude (stick out) from the side of the foot, at the base of the big toe. If this happens, a painful, swollen bunion forms. It is not known exactly why bunions occur, but wearing badly fitting shoes is thought to be a possible cause. If bunions become worse over time they can cause other problems, such as arthritis within the big toe joint. Surgery for a bunion may be advised if simple measures such as well- fitting shoes, pain relief and padding do not relieve the discomfort.
The operation may also be performed if the big toe is so deformed that it is pressing on or overlapping the second toe (hallux valgus).
Surgery is only appropriate if you are willing to adapt your footwear as instructed after surgery and understand and accept the potential risks of the procedure.
What does the operation involve?
A cut is made on the side of the bunion then the big toe joint is opened and the bony lump (bunion) is removed. The first bone (metatarsal) is cut through; it is then repositioned and fixed with 1 or 2 screws. The bone at the base of the big toe (phalanx) may also be cut. Sometimes another cut is made between the first and second toes to free up the tight tissues on the side of the toe. The soft tissues (e.g. muscles, tendons and ligaments) on the other side of the joint are tightened to correct the deformity and the wound stitched up. The foot is dressed in soft bandages.
Is this a day case operation?
Yes. The operation is often done on a day case basis if you are medically fit, able to walk with crutches after the operation and have someone who can collect you and look after you when you are at home.
If you have other medical problems such as diabetes, asthma or high blood pressure you may have to attend the Preoperative Assessment Clinic 2 to 6 weeks before your surgery.
You may stay in the hospital after the operation if your foot is not comfortable. Local anaesthetic injections may help with this.
Will I have a general anaesthetic?
Your anaesthetist will advise about the best choice of anaesthetic for you. The operation can be performed under general anaesthetic (while you are asleep) or occasionally, an injection in the back or leg (local anaesthetic) can be given to make the foot numb. If you are given a local anaesthetic you will you remain awake for the operation.
Local anaesthetic may be injected into your leg or foot during the operation to reduce the pain after the operation. You will also be given pain relief as needed after the operation.
Will I have a plaster cast on afterwards?
You do not usually need a plaster cast after a metatarsal osteotomy. Instead you will have it dressed appropriately in bandages and a walking shoe that only allows you to bear weight through your heel. This is called a Darco shoe. After 2 weeks, the stitches are removed and a splint is used to hold the big toe in the corrected position for a further 4 weeks. You would usually wear the splint for 6 weeks.
If your bone is particularly soft or the soft tissue repair of the joint needs extra protection, a plaster will be put on.
Going home
You can go home when you are comfortable and safe. A therapist will show you how to walk safely with crutches and advise on going up and down the stairs. For the first 2 weeks, you should avoid walking if possible and only put your weight through the heel. Rest with your foot elevated to reduce any swelling. An X-ray may be taken before you go home.
Follow up appointment
You will be seen by a nurse or doctor in a clinic 14 to 17 days after your operation; this appointment may be given to you on the ward or posted to you after your discharge home. The dressings will be removed, the wound examined and any stitches removed. An X-ray may also be taken.
A splint will be put on your toe to hold it in position so that you will be more mobile and able to walk on your heel using crutches for support. You can remove the splint for bathing and showering.
Another clinic appointment will be made for 4 weeks later. At this appointment the splint will be removed if the wound has healed. If the wound has not healed enough you may need to continue using the Darco shoe for another week or two.
After 3 months another X-ray is taken. If this shows the osteotomy has joined, you can return to normal activities.
Planning for your operation
We recommend that you plan in advance how you are going to manage at home after the operation. This is particularly important if you live alone. Stock your freezer and cupboards as getting to the shops will be awkward and tiring at first. You will need to use a waterproof cover to protect the plaster cast if using the shower. Some people have both feet operated on at the same time. In these cases, hiring a wheelchair is a good option. Details can be found at the end of this page.
Further advice
Walking
For the first 2 to 4 weeks you should walk with the crutches and the Darco shoe as advised by the therapist. This involves weight bearing through the heel only.
When you are not walking you must rest with your foot elevated as much as possible to reduce swelling. After this period you can be more mobile but you must still walk putting your weight through the heel.
Going back to work?
This depends on what you do and how you get to work. If you can be taken and collected from work and you have a sitting-down job that you could do with your foot in bandages or a splint, you can return to work about 3 weeks after surgery. If you have a heavy manual job you may be away from work for up to 3 months. Your surgeon or foot and ankle nurse will advise you about going back to work.
Driving
Once your splint has been removed you may be able to start driving again. You must be comfortable and not too stiff before trying to drive. Start by sitting in the car and pressing the pedals then drive a short distance. You should only drive short distances at first. If you cannot safely make an emergency stop your insurance will not cover you in the event of an accident. Most people are able to perform an emergency stop between 6 and 8 weeks after surgery.
Playing sport
After your splint has been removed, you can start gently exercising your foot and walking further each day. When you are comfortable doing this you can start gentle running and stretching. Everyone varies as to how quickly they can take up exercise again; be guided by your own body’s reactions and the advice of your surgeon.
Most people can get back to most of their previous activities within 6 months of bunion surgery.
Risks
- Swelling. It is normal for your foot to swell after surgery. It may take up to 6 months for the swelling to disappear
- The big toe is often stiffer than before you had the surgery. For most people this does not cause any problems
- Metatarsalgia. This is where you feel pain under the ball of the foot. Careful surgical technique can reduce the risk of developing metatarsalgia but cannot avoid it completely. Most people who develop metatarsalgia are comfortable with a simple insole in the shoe but occasionally further surgery is needed. The big toe is slightly weaker with a bunion and this transfers weight onto the ball of the foot; after bunion surgery, this transfer of weight can increase
- Recurrence of the bunion. Occasionally overtime, the big toe may move back to the original position and you may need to have further investigations
- Infections in the wound and minor damage to the nerves of the toe can happen in any foot surgery. Usually, these are minor problems that get better quickly
- Deep Vein Thrombosis (DVT) and Pulmonary Embolus (PE) (blood clots in your legs and lungs)
Contact information
Red Cross
For wheelchair loans
Tel: 01452 726666
Limbo
Waterproof shower protectors for plaster casts
Tel: 01243 573 417
Social Services
Helpdesk
Tel: 01452 426 868
Further information
The British Orthopaedic Foot Surgery Society web site is available at:
Website:
www.bofas.org.uk/PublicArea/PatientAdvice/tabid/85/Default.aspx