Rectal cancer
This page is for patients diagnosed with a cancer in the rectum (back passage). The information will help you to understand the patient pathway, and make you aware of the various treatment options that might be available to you.
On this page
-
What is rectal cancer?
-
Diagnosis
-
Investigations
-
The Multidisciplinary Team (MDT)
-
Treatment
-
Pre-operative radiotherapy and chemotherapy
-
Staging of rectal cancer
-
TNM staging system
-
Post-operative radiotherapy and chemotherapy
-
Clinical trials
-
What if my cancer has spread?
-
Palliative treatment
-
Patient support
-
Contact information
-
Further information
What is rectal cancer?
The tissues and organs of the body are made up of cells. Cells age and become damaged and need to repair and reproduce themselves continuously. When this process gets out of control, the cells reproduce and multiply to form an abnormal mass (or tumour). Tumours can be benign (not cancerous) or malignant (cancerous). A malignant tumour consists of cancer cells that can spread to other organs in the body. Rectal cancers are very common. They often develop from a growth known as a polyp, which usually start as benign tissue and over a period of time can turn cancerous. If this is caught early enough, many rectal tumours can be removed. The most common type of rectal tumour is an adenocarcinoma.
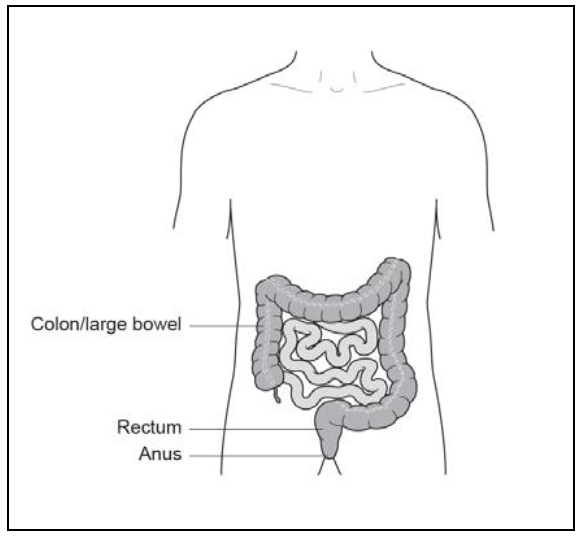
The diagram (Figure 1) indicates where the cancer (proven or suspected) is located in your body.
Diagnosis
A diagnosis of rectal cancer is proven by taking a biopsy (tissue sample) from the tumour and examining it under the microscope. A biopsy may either be taken by having a proctoscopy (a thin tube put into your back passage to examine the anal canal and rectum), or by having a flexible sigmoidoscopy or colonoscopy (as described on this page).
Investigations
To help us decide how to treat the cancer it is very important that we get the necessary information about the cancer and the rest of your body.
This is called ‘staging investigations’ and can involve several tests which may include:
Computerised Tomography (CT) scan
CT is a detailed X-ray examination of the body. It is used to look for abnormalities and in particular to see if there is any evidence that the cancer may have spread.
Magnetic Resonance Imaging (MRI) scan of your pelvis
MRI is a scan using magnetic waves to create images of the body and will give a detailed picture of the tissues of the rectum and pelvis. This information will help the specialists to decide on the best form of treatment for you.
Colonoscopy or flexible sigmoidoscopy
Colonoscopy or flexible-sigmoidoscopy tests both use a flexible tube with a light and a camera, and will give a clear idea of what the tumour looks like. A colonoscopy visualises the whole of the colon, whereas a flexible sigmoidoscopy is limited to views of the left side of the colon. These procedures can be used to take a biopsy of the tumour, and to mark the area with a tattoo if you are going to be offered keyhole (laparoscopic) surgery. A colonoscopy also gives an opportunity to view the rest of the colon to check that there are no other tumours or polyps.
Trans Rectal Ultrasound (TRUS)
The tumour will be scanned through the back passage. The tumour and the surrounding tissue will be assessed.
Carcino Embryonic Antigen (CEA) blood test
CEA is a tumour marker blood test which is used to measure the amount of chemical substance produced by a cancer. It can help to give some information about the type and extent of the cancer.
The Multidisciplinary Team (MDT)
All of your results will be discussed at a colorectal cancer specialist multidisciplinary team meeting. This meeting takes place once a week and is attended by consultant colorectal surgeons, a consultant radiologist, a consultant histopathologist, a consultant clinical oncologist, colorectal clinical nurse specialists and other members of the colorectal team.
At this meeting the specialist team will use their expertise to determine what will be the most effective and appropriate form of treatment for you.
It may be possible to keep you up-to-date with the outcomes of the MDT meetings. The colorectal nurse specialist may contact you, if appropriate, and has previously been agreed with you.
Treatment
The treatment offered to you will be dependent upon the results of your staging investigations, your general health and other medical conditions. You will be offered an appointment with your consultant to discuss the treatment options open to you. You will be actively involved in any decision making and your views and wishes will be respected at all times.
Bowel resection
The primary treatment for rectal cancer is an operation to remove the part of the rectal containing the cancer. The operation that you require will depend on exactly where the cancer is and the information provided by your staging scans.
In most cases, rectal cancers can be removed and the bowel joined back up. However, it is sometimes necessary to make a temporary stoma (usually an ileostomy) to allow the join in the bowel to heal. An ileostomy is made by bringing a loop of the small bowel up to the surface of the abdomen where it is stitched in place and faces (stools) will be passed into a bag which covers it. A temporary ileostomy is usually reversed after a minimum of 3 months.
If a rectal cancer is very low down in the back passage it may be necessary to remove the entire back passage and make a permanent stoma. This type of stoma would be a colostomy which is formed from the large bowel.
If surgery is planned, you will normally be given a leaflet explaining the operation.
Transanal Endoscopic Microsurgery (TEMS)
This allows surgery to be performed within the rectum using a specialist microscope. There are usually no external incisions or scars. This technique is only used to remove small cancers from the rectum either because the cancer is very early or because your consultant feels that you are not medically fit to have major surgery.
Pre-operative radiotherapy and chemotherapy
Radiotherapy is the use of controlled, high-energy radiation, usually X-rays to destroy cancerous tumours.
You may be offered radiotherapy before surgery which will:
- Shrink the tumour in order to make it easier to remove
- Reduce the risk of cancer coming back (recurrence) after your surgery
This treatment will either be a short course (5 treatments over 5 days) or a long course (5 treatments a week for 5 or 6 weeks). The length of treatment depends on the stage of your tumour. Long course radiotherapy is usually given at the same time as chemotherapy, as this makes the cancer cells more sensitive to the radiation. Chemotherapy is the use of ‘anti-cancer’ (cytotoxic) drugs to destroy cancer cells in the body.
Staging of rectal cancer
The exact stage of a colon cancer can often only be determined after surgery, when the pathologist can examine the cancer and the piece of healthy colon that has been removed.
The TNM staging system is used to stage colon cancer.
TNM staging system
Tumour
Describes the tumour and how far it has invaded through the bowel wall.
Nodes
Describes whether the cancer has spread to the lymph nodes.
Metastases
Describes whether the cancer has spread to another part of the body such as the liver or lungs.
Post-operative radiotherapy and chemotherapy
Depending on the stage of your tumour you may be offered a course of chemotherapy after your operation. This is also called an adjuvant treatment. The chemotherapy is used to destroy cancer cells in the body that remain after the tumour has been removed by surgery. It will also reduce the possibility of the cancer returning.
If radiotherapy was not given before surgery, you may be advised to have a course of radiotherapy with the chemotherapy:
- To destroy any cancer cells that may be left behind
- If the tumour was difficult to remove
- If your cancer has grown through the wall of the rectum or spread to nearby lymph nodes
Clinical trials
There are a number of current clinical trials relating to treatments for rectal cancer. If you are eligible to take part in any of these trials, this may be discussed with you by an oncologist or a clinical trials nurse.
What if my cancer has spread?
Sometimes rectal cancers can spread to other organs in the body, most commonly the liver, lungs and peritoneum (lining of the abdominal cavity). This is known as secondary cancer or metastases.
If this is shown to be the case on your staging scans, the treatment which can be offered will be dependent on the extent of the metastases.
In some circumstances it may be possible to offer surgery or other specialist therapies to treat metastases. These operations and therapies are not performed by the Gloucestershire Hospitals NHS Foundation Trust so patients would be referred to other specialist units.
Palliative treatment
If the spread of the cancer to other organs is extensive, you have decided to decline surgery or you are medically unfit for major surgery, then you may be offered palliative radiotherapy and/or chemotherapy. This may help to control your symptoms and slow down the progression of the disease, but this will not be a cure.
Stenting
This is the insertion of a stent which is a flexible hollow tube that can be rolled up tightly and passed through the tumour. Once in place, stents are able to expand to keep the bowel open and prevent blockages. Stenting is subject to the position of the tumour.
Formation of a stoma
If it is not possible to offer you an operation to cure your cancer, but you are getting a lot of adverse symptoms from your bowel being narrowed, you may be offered an operation to form a stoma. This may either be an ileostomy (formed from the small bowel) or a colostomy (formed from the large bowel). The aim would be to bypass the blockage and relieve your symptoms.
Best supportive care
If you are not medically fit to have any of the described treatments or you decide to decline treatment then you will be offered palliative or best supportive care. This is a treatment plan to relieve your symptoms and to enhance your quality of life for as long as possible.
Patient support
Being diagnosed with colon cancer will come as a shock to most people. As you progress through your treatment pathway you are likely to experience a rollercoaster of emotions, and you will have lots of questions and concerns, and often some difficult decisions to make.
You will meet one of the colorectal nurse specialists who will be your keyworker.
Your keyworker is there to support you through your treatment pathway. They will be happy to speak to you if you want an explanation of any of the information you have been given, if you need advice or if you are simply having a bad day and need someone to lend a sympathetic ear.
Further appointments to meet with your consultant will also be made as necessary.
Contact information
Colorectal Nurse Specialist
Cheltenham General and Gloucestershire Royal Hospitals
Tel: 0300 422 5617
Monday to Friday, 8:00am to 4:00pm
Outside of these hours, please leave a message and someone will return your call the next working day.
Stoma Nurse Specialist
Cheltenham General Hospital
Tel: 0300 422 4363
Monday to Friday, 8:00am to 4:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 6702
Monday to Friday, 8:00am to 4:00
Outside of these hours, please leave a message and someone will return your call the next working day.
Further information
Macmillan Cancer Support
Tel: 0808 808 00 00
Monday to Friday, 9:00am to 8:00pm
Website: www.macmillan.org.uk
Bowel Cancer UK
Website: www.bowelcanceruk.org.uk
FOCUS Cancer Information Centre
Cheltenham General Hospital
Tel: 0300 422 4414
Monday to Friday, 8:30am to 4:30pm
Maggie’s Centre
College Baths Road, Cheltenham
Tel: 01242 250 611
Monday to Friday, 9:00am to 5:00pm
‘Mini’ Maggies
The Main Place, Old Station Way, Coleford GL16 8RH
Tel: 01242 250611
Offering practical and emotional support, facilitated and peer support groups as well as fitness and relaxation classes. Sessions run on the third Friday of each month from 10:00 am to 2:00 pm.
Macmillan Information Hub
Gloucestershire Royal Hospital
To access the service either drop in (no appointment needed) or call:
Tel: 0300 422 8880
Email: ghn-tr.macmillanhub@nhs.net
Monday to Friday, 9:00am to 4:00pm