Reversal of Hartmann’s procedure
This page gives you information about the reversal of Hartmann’s procedure. It explains what the procedure involves and some of the common problems that patients may experience with it.
On this page
-
The digestive system
-
What is a reversal of Hartmann’s procedure?
-
Benefits of the procedure
-
Bowel habit
-
What is keyhole surgery?
-
Possible risks and complications of having this procedure
-
What are the alternatives to this procedure?
-
How long does the operation take?
-
How long will I be in hospital?
-
Pre-operative, post-operative and discharge advice
-
What follow-up care will I have?
-
Contact information
In the past, you will have had an operation which removed part of your large bowel (the sigmoid colon).
At the time of your operation, it was not possible to re-join your bowel. Your rectum (back passage) was sealed off inside you and the upper part of your large bowel was brought out to the skin on your abdominal (tummy) wall as an open end of bowel – known as a colostomy. Some time for healing has passed and it has been recommended that you now have surgery to reverse the colostomy which was formed after your operation.
We recommend that you read this page carefully. Please ask your surgical team about anything you do not fully understand or want explained in more detail.
The digestive system
To understand your operation, it is helpful to have a basic knowledge of how the body works (see Figure 1).
When food is eaten, it passes from the mouth down the oesophagus (food pipe) and into the stomach. The food is broken down and becomes semi-liquid. It then continues through the intestine (small bowel), which is many feet long, where the food is digested and nutrients are absorbed.
The semi-liquid food then passes into the colon (large bowel) and becomes faeces (stools). The main job of the colon is to absorb water into our bodies making the stools more solid. The stools then enter a storage area called the rectum. When the rectum is full, we get the urge to open our bowels.
Figure 1: Digestive tract
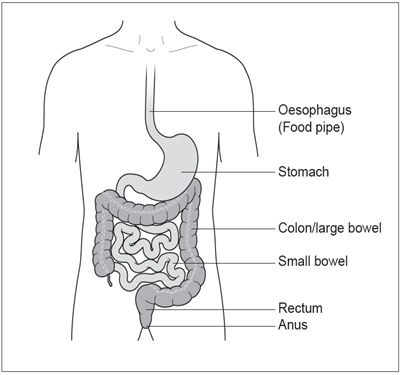
The stools are finally passed through the anus (back passage) when we go to the toilet.
What is a reversal of Hartmann’s procedure?
The procedure now will be to re-enter your abdominal cavity (usually through the original scar), cut around the colostomy to free it from the skin and the abdominal wall muscles. The surgeon will then join up the bowel to the remaining rectum, either using special stapling instruments or sutures (stitches). This means you should be able to use the toilet in the normal way. Your wound will be closed with stitches, including the hole where the colostomy was. Your bowel function may not fully return to normal after this operation and you may have looser stools or need to empty your bowels more often than usual.
Depending on where the join of your bowel is, you may need a different temporary ‘bag’ (known as an ileostomy). Your consultant will talk with you about this before the operation. You will also see the stoma nurses who will discuss the differences between looking after an ileostomy and a colostomy.
Your doctor (or other health professional) will need to have, in writing, that you agree to have the procedure so you will be asked to sign a consent form.
Benefits of the procedure
The aim of the surgery is to restore and enable your bowel to function normally. For most patients, this will result in a much better bowel function because they will no longer have the colostomy.
Bowel habit
Your surgery re-joins the part of the bowel which normally stores waste material. Many patients have constipation or diarrhoea (or both) for some time after the operation. Some patients may also have some ‘urgency’ to empty the bowel and may feel the need to pass small stools more often than normal. How long this continues will vary from patient to patient.
What is keyhole surgery?
Keyhole surgery involves carrying out an operation through small cuts in the abdomen, rather than one large cut. The surgeon will put a narrow telescope attached to a camera and other special instruments through the cuts to re-join the ends of the bowel.
The decision about whether to use open (large cut) or keyhole surgery will be made after a discussion between you and your surgeon. Your surgeon will consider whether your condition is suitable for keyhole surgery, together with the risks and benefits of both procedures.
The benefits of keyhole surgery include:
- A shorter hospital stay.
- Less pain after surgery.
- A smaller scar.
The possible risks of having keyhole surgery are the same as for open surgery. If for technical reasons it is not possible to complete your operation using keyhole surgery then the surgeon would need to change to an open operation. This will be discussed with you during the consent process.
Possible risks and complications of having this procedure
Re-joining part of the bowel is a major operation. Risks with this operation include:
Anastomotic leak
The join in the bowel (known as anastomosis) can sometimes leak. Treatment with antibiotics and resting the bowel are usually enough to resolve this problem. A leak is a serious complication, if it is not resolved with antibiotics and resting the bowel, further surgery and the creation of a new stoma may be needed.
Ileus (paralysis of the bowel)
The bowel is slow to start working after surgery and this can cause vomiting and stop you from eating and drinking normally. If this happens the bowel may need to be rested and a drip (a tube into a vein in your arm) is used to replace fluids (instead of drinking).
You may also need a nasogastric tube (tube in your nose which passes into your stomach) so that the fluid collecting in your stomach can be drawn off. This helps to stop the nausea and vomiting and will stay in place until the bowel recovers.
Adhesions (scar tissue)
With any abdominal surgery, some scar tissue is formed. This is known as adhesions. For some people, this can lead to further problems which may need more surgery, but this is rare.
After any major operation there is a risk of:
Chest infection
- You can help by practicing regular deep breathing exercises and following the instructions from the physiotherapist. If you smoke, we strongly advise you to stop.
Wound infection
- If your wound becomes infected, this is usually not serious but may need treatment. You may be given antibiotics or if there is a collection of fluid, this may need to be drained to allow your wound to continue to heal.
Thrombosis (blood clot in the leg)
- Major surgery carries a risk of a blood clot forming in your leg. To lower this risk, a small dose of blood thinning medication will be given daily, by injection, until you go home. You will also be fitted with support stockings to be worn during your hospital stay. You can help by moving around as much as you are able to and by exercising your legs.
Pulmonary embolism (blood clot in the lung)
- Rarely, a blood clot from the leg can break off and become stuck in the lungs. This would need treatment with blood thinning medication.
Bleeding
- A blood transfusion may be needed during or after your operation. Very rarely, further surgery may be needed if the bleeding continues after your operation.
Risk to life
- Surgery to re-join part of the bowel is classed as major and can carry a risk to your life. Your surgeon will discuss this risk with you during the consent process.
Most people will not have any serious complications from their surgery. Risks increase with age and for those who already have heart, chest or other medical conditions such as diabetes or for those who are overweight or smoke.
What are the alternatives to this procedure?
Deciding not to have the reversal of Hartmann’s procedure will mean you will be left with your stoma permanently. Your surgeon will answer any question you may have and discuss any queries with you.
How long does the operation take?
This operation usually takes between 1½ and 2 hours but you will be away from the ward for a longer period of time. You will spend time in the recovery area after your operation. When you are fully awake, feeling comfortable and your general condition is stable, you will be taken back to the ward.
How long will I be in hospital?
From the start of your hospital stay, you will be following an ‘enhanced recovery programme’ which aims to help you recover quicker and safely. We usually say that you should be ready for discharge within 5 to 7 days if there are no problems with your recovery.
Pre-operative, post-operative and discharge advice
For further information about what to expect when you come into hospital, what your recovery will involve and for discharge advice, please refer to your information booklet ‘Enhanced Recovery Programme’ (reference number GHPI0815).
What follow-up care will I have?
Following discharge from hospital, your colorectal nurse specialist will give you the contact details for the team so that you have direct access. Please contact the team if you have any concerns about your immediate recovery on your return home.
You will be seen at an outpatient appointment about 6 weeks after your discharge. Your consultant or one of the colorectal nurse specialists will assess how well you are recovering from your operation and check your wounds.
If your operation was for cancer, your consultant or colorectal nurse specialist will also discuss your follow-up care with you, known as your individualised ongoing surveillance programme.
If a new stoma was formed, the stoma nurse specialist will telephone you about a week after your discharge to plan a home visit to check the stoma.
Contact information
If you need further advice or information, your colorectal nurse specialist or stoma nurse specialist will be happy to speak to you. Please use the contact numbers provided below.
Colorectal Nurse Specialist
Cheltenham General Hospital
Tel: 0300 422 5617
Monday to Friday, 8:00am to 4:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 5617
Monday to Friday, 8:00am to 4:00pm
Outside of these hours, please leave a message when prompted. Your call will be returned the next working day.
Stoma Nurse Specialist
Cheltenham General Hospital
Tel: 0300 422 4363
Monday to Friday, 9:00am to 4:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 6702
Monday to Friday, 9:00am to 4:00pm
Outside of these hours, please leave a message when prompted. Someone will return your call the next working day.
If your problem is urgent, the team can be contacted via the hospital switchboard:
Gloucestershire Hospitals Switchboard
Tel: 0300 422 2222
When prompted, ask for the operator then for the Colorectal Nurse Specialist or the Stoma Nurse Specialist.