Flexible sigmoidoscopy as an outpatient
You have been advised to have a flexible sigmoidoscopy to investigate the cause of your symptoms. It is important that you read this page before your appointment so that you understand what will happen during the procedure and any preparations needed.
Medication
You must stop taking any medicines containing iron 7 days before your appointment.
If you have diabetes and you are receiving treatment, please leave a message on the Medication Advice Line. The number is at the end of this page. If you use an insulin pump, we would like your BM to be 7mmol/L. Please call your local pump team if you need advice.
If you are taking any medication that thins your blood other than aspirin (which you can remain on) or you are pregnant, please ask your GP or referring consultant for advice. Alternatively, you should call the Medication Advice Line.
Your procedure may be delayed if you do not obtain advice.
What is a flexible sigmoidoscopy?
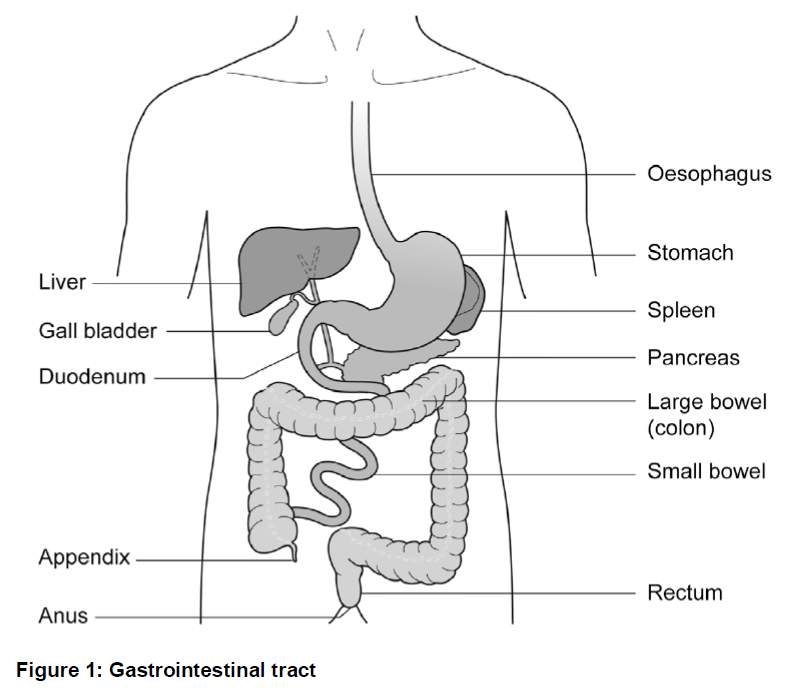
Flexible sigmoidoscopy is a test which allows the doctor to look at the lower part of your large bowel (sigmoid colon). A flexible colonoscope is passed through the anus (back passage) and into the bowel.
A colonoscope is a flexible tube about the thickness of your index finger with a bright light on the end. By looking at the screen, the doctor can see the lining of the bowel and check whether any disease is present.
Biopsy
Sometimes the doctor will take a biopsy, a small sample of tissue, to be examined in the laboratory.
It is also possible to remove polyps during the flexible sigmoidoscopy. Polyps are abnormal bits of tissue, like warts, which the doctor will want to examine in more detail in the laboratory. This procedure will not be painful.
Alternative procedures
The main alternative to this test is a barium enema X-ray and CT scan. This procedure can look at the sigmoid colon but does not allow biopsies to be taken or look directly at your bowel. The alternatives will not be available on the day of your test.
Preparation for your procedure
Your bowel must be cleaned and empty for this test. The endoscopy department will send you a bowel preparation through the post. Full instructions will be given.
If you do not receive a preparation ring the booking team urgently.
The telephone number is at the end of this page.
If you are sent an enema, you may eat and drink normally until the enema is inserted.
Do not eat any solid food after you have inserted the enema.
Continue to take any medicines prescribed by your doctor unless you have been told otherwise.
The NHS, a major contributor of carbon emissions in the UK, has recently outlined ambitious targets to achieve net zero carbon emissions by 2040. The endoscopy team in Gloucestershire have carefully considered ways of adopting more sustainable care and waste reduction.
We would appreciate your support to help make our practice ‘greener’ by kindly bringing the following items along to your endoscopy appointment, so that single use alternatives are not required:
- Dressing gown
- Pair of slippers
- Clean underwear to change into after the procedure
- If applicable, your own denture pot, hearing aid case(s) and/or eye glasses case
- Water bottle
- Reusable cup with lid for a complimentary hot drink after the procedure
- Bag to place your clothes in during procedure
On admission
You will be seen by a nurse who will check your personal details, allergies and medical history.
Please bring with you to your appointment a list of the medication you are currently taking (including sprays and inhalers).
You will be asked to sign a ‘Consent Form’ to agree to have the test done. This does not take away your right to ask for the test to be stopped at any time.
You will then be asked to change into a hospital gown.
A small enema will be given to clear the bowel, unless you have done this at home.
You will have received the enema on this page. If you are able to give yourself the enema at home you will not need another. If you are unable to do so, please bring the enema with you and a nurse will help.
The toilet will be easily accessible, or a commode can be put next to your bed if you prefer.
For the time that you are in the department we want to provide a safe, supportive and pleasant environment so please do not be afraid to ask if you have any worries or questions at this stage.
Please remember that your appointment time is not the time you will have your investigation. There will be a wait between your admission and having your test done.
The test and potential complications will be explained to you so that you understand the procedure and any risks involved.
You will be shown into the room where your sigmoidoscopy will take place. You will be made comfortable on a patient trolley, lying on your left side with your knees slightly bent. A nurse will stay with you throughout the procedure.
During the test
- A rectal examination may be done as part of the procedure. This is where a doctor uses their finger to check for any problems inside your bottom (rectum). This is usually very quick and you should not feel any pain.
- When the tube has been gently inserted through your anus into the large bowel, air will be passed through it to give a clear view of the lining. This may give you some wind like pains but will not last long.
- You may also get the sensation of wanting to go to the toilet. As the bowel is empty, there is no danger of this happening. You may pass some wind but please do not be embarrassed.
- Sometimes a nurse will assist the endoscopist by applying some pressure to your abdomen (tummy) with their hand. This can often help the endoscope to progress through your bowel more efficiently.
- The test usually takes between 5 and 10 minutes. When the test is finished, the tube is removed quickly and easily. Most of the air put in during the test will be taken out as the tube is removed.
- As this is a quick procedure, sedation (medicines to make you sleepy) is not normally given. However, if you did want sedation, this is available providing you have someone to take you home and a responsible person to be with you for 24 hours following the procedure.
- Entonox® (nitrous oxide) is now available in all units for pain relief; please ask your admitting nurse if this is an option for you.
Intravenous sedation (optional)
The sedation will be given into a vein in your hand or arm. This will make you slightly drowsy and relaxed but not unconscious. You will be in a state called conscious sedation which means that, although drowsy, you will still hear what is said to you and will be able to follow simple instructions. Sedation makes it unlikely that you will remember anything about the procedure. You will be able to breathe normally throughout.
While you are sedated your breathing and heart rate will be checked regularly. A probe connected to your finger will measure your oxygen levels and heart rate during the procedure. Your blood pressure will also be recorded.
Please note that if you decide to have sedation you should not drive, drink alcohol, operate heavy machinery or sign any legally binding documents for 24 hours following the procedure. You will need someone to accompany you home and stay with you for 24 hours.
Entonox® (gas and air) is also available during the procedure either as an alternative to sedation or as well as. This will help to control any discomfort. You will not need a responsible adult to stay with you if you choose Entonox® only. (A separate leaflet has been provided).
If you have experienced or suffered with any of the following within the last 12 weeks, Entonox® will not be suitable for you.
- Pneumothorax
- Air embolism
- Emphysema/COPD
- Recent ear/eye surgery
- Head injury with impaired consciousness
- Bowel obstruction
- Scuba diving
- Decompression sickness
Risks associated with having sedation
Sedation can sometimes cause problems with breathing, heart rate and blood pressure. To reduce these risks, you will be monitored during the investigation. Older patients and those who have health problems, for example, people with breathing difficulties due to a bad chest, may be assessed by a doctor before being treated.
Complications
Complications are uncommon. If a biopsy is taken or a polyp removed it can lead to bleeding or a perforation (a tear) in the bowel. Bleeding usually settles on its own. A perforation may need major surgery. However, the risk a complication such as this is small. The overall complication rate including perforation and bleeding is less than 1 in 20,000 cases.
After the test
After the sigmoidoscopy is completed, the nurse caring for you during your test will take you from the Endoscopy room and into the recovery area. You then be able to get dressed and go home.
It is common to feel slightly bloated with wind for a short time after the test.
If a sample (biopsy) has been taken, the result will take up to 5 weeks to process. You may be given an outpatient’s appointment to return for review or the result will be forwarded to your GP.
Going home
If you have had sedation, it is essential that someone takes you home and that there is a responsible adult to stay with you for 24 hours.
You can go home by taxi but you must have someone to accompany you on the journey. For this period of time, you should not:
- Drive a car, ride a motorbike or a bicycle.
- Drink alcohol.
- Operate machinery or do anything requiring skill or judgment.
- Make important decisions or sign any documents.
If you did not have sedation the above paragraph does not apply.
If you have received Entonox® for pain relief, you will need to stay in the department for 30 minutes before going home.
An advice sheet will be given to you before you leave the department. This is also your discharge letter. A report of the procedure will automatically be sent to your GP.
If you have a polypectomy (polyp removed from your bowel), there is a risk of delayed bleeding. If the polyp is large or there are lots to be taken away, it is important to let your endoscopist know if you intend to travel (especially long-haul flights) in the days following this treatment.
Gloucestershire Hospitals NHS Foundation Trust Endoscopy Units are training centres. Registrars and nurse endoscopists regularly attend endoscopy lists.
If you have any concerns, please discuss with the admission nurse.
Contact information
Appointment Enquiries
Tel: 0300 422 6350
Tel: 3000 422 6351
Monday to Sunday, 8:30am to 4:00pm
Medication Advice Line (Answer Machine)
If you have any questions relating to your medication, please leave a message. A member of staff will return your call normally within 24 hours, week days only.
Cheltenham General Hospital
Tel: 0300 422 3370
Monday to Friday, 8:00am to 6:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 8232
Monday to Friday 8:00am to 6:00pm
Saturday and Sunday, 9:00am to 12:00 midday
Other Endoscopy Units
Cirencester Hospital
Tel: 0300 421 6294
Monday to Friday, 8:00am to 4:00pm
Stroud General Hospital
Tel: 0300 421 8073
Monday to Friday, 8:00am to 6:00pm