Urinary Tract Infection
This page gives you information about Urinary Tract Infections (commonly known as a UTI) and how they can be treated, managed and prevented. Also included are the common symptoms of UTI’s.
On this page
-
What is a Urinary Tract Infection (UTI)?
-
What causes a UTI?
-
What are the symptoms of a UTI?
-
How to try to prevent a UTI (self-help)?
-
What should you do if you suspect you have a UTI?
-
When to seek medical advice from your GP or NHS 111
-
What medical treatment is available?
-
Treating a recurrent UTI
-
Alternative treatments in preventing a UTI
-
Further investigations
-
Contact information
-
Further information
What is a Urinary Tract Infection (UTI)?
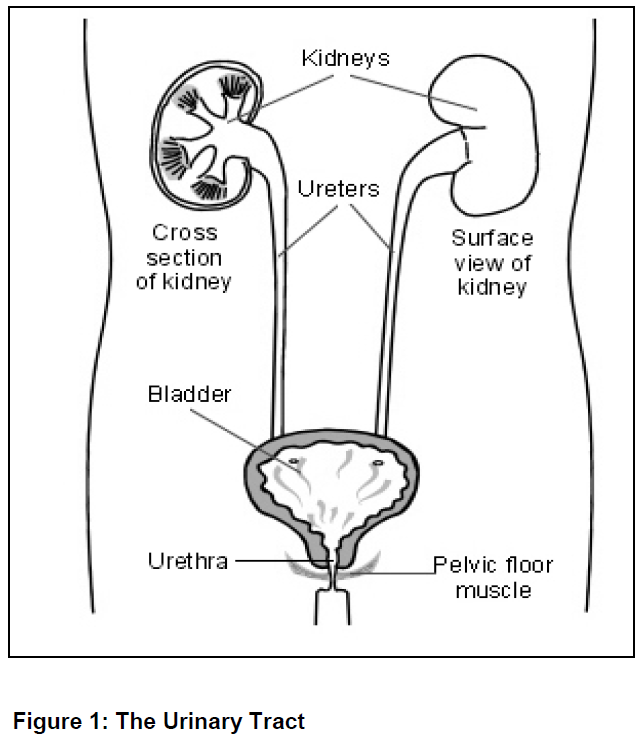
A UTI is an infection within the urinary system. The infection can be in the kidneys, ureters, bladder or urethra (waterpipe). Infections affecting the urinary tract are very common and affect most women at least once in their lifetime. Up to 1 in 5 women will have problems with repeated infections. They occur at any time but are most likely in women who are sexually active, pregnant or have been through the menopause.
What causes a UTI?
UTI’s are usually caused by bacteria entering the urethra and moving up into the bladder. The most common bacteria causing a UTI is E. coli (Escherichia coli).
E.coli is essential for a healthy bowel (colon) but is often spread when people open their bowels. It happens more often in women because the opening of the bottom (anus) is so close to the opening for urine to exit (urethra). The urethra in women is shorter than that in a man which makes it easier for the bacteria to access the urinary tract.
Factors which can increase the possibility of having a UTI:
- Not drinking enough fluids. You should aim to drink 8 glasses of fluid every day to prevent dehydration.
- If you drink regular alcohol, this causes dehydration which increases the risk of a UTI.
- Medicines or conditions which weaken your immunity, for example diabetes.
- Pregnancy.
- Having a urinary catheter.
- The bladder not emptying completely, such as in men with an enlarged prostate and in women with a uterine (womb) or bladder prolapse.
- Other conditions which block the urinary tract, for example, kidney stones.
What are the symptoms of a UTI?
Many people have little or no symptoms but some experience the following changes:
- Dehydration which includes dry mouth or lips, being thirsty, tiredness, headaches, dry skin and dark coloured or strong smelling urine.
- The need to pass urine often; perhaps as often as every ½ hour.
- A sudden need to pass urine known as urgency.
- Burning/stinging when you pass urine.
- Passing cloudy urine.
- Being incontinent of urine, when normally you are not.
- Blood in your urine.
- Tenderness or pain in the lower part of your abdomen.
When the infection is more severe you may experience:
- Pain in your back or side (particularly under the ribs, and in the area where your kidneys are.
- A high temperature above 38C.
- A very low temperature below 36C.
- Feeling shivery or shaking uncontrollably, feeling hot then cold
- Feeling of being cold /clammy skin.
- A sudden onset of confusion or agitation, particularly in an older person.
- Not passed urine all day.
- Feeling short of breath.
- Sickness (nausea or vomiting).
Please seek medical advice and call NHS 111 - these symptoms suggest a kidney infection and can be serious if not promptly treated.
How to try to prevent a UTI (self-help)?
Drink plenty of fluids. Aim to drink at least 8 glasses of fluid every day to prevent dehydration. In warmer weather the risk of developing a UTI increases so you should increase your fluid intake. Alcoholic drinks can also cause dehydration.
Always check the colour of your urine; if your urine is a dark orange/brown (strong) you need to drink more. Be aware of how much urine you are passing at each time. If you are passing small amounts, increase the amount of fluids you are drinking. Your urine should be a pale yellow colour.
If you struggle to drink fluids try adding water based foods to your diet such as, jellies, ice-lollies, soups, melons, cucumbers, tomatoes, strawberries, peaches, oranges, grapefruit, lettuce, cauliflower, cabbage, skimmed milk, plain yogurt, cottage cheese. See leaflet ‘Fluid and caffeine intake for bladder and bowel health’ GHPI0533.
Other simple lifestyle changes:
- Wiping from front to back after you go to the toilet to prevent bacteria entering your urethra.
- If you experience constipation this can increase the risk of UTI so see the leaflet mentioned above for further information.
- Allow yourself time on the toilet to empty your bladder fully.
- Wear loose cotton underwear, avoid wearing tight fitted synthetic underwear, tights and tight trousers made from man-made fabrics i.e. nylon material.
- Take a shower rather than a bath.
- Avoid waiting too long to go to the toilet, as this can hold the bacteria in the bladder.
- Sexual hygiene - passing urine and washing gently with warm water after sex can help reduce the amount of bacteria present.
- Avoid constipation.
- Avoid soaps, shower gels and intimate hygiene products (wet wipes or talcum powder); these can irritate the urethra.
- Incontinence - treating the incontinence, whether urinary or faecal, can help to reduce the risk of UTI.
Leakage of urine as women get older is not just as part of ageing. Wearing pads to cope with incontinence can increase your risk of UTI so if you are suffering with this you may want to talk to your GP or nurse about addressing the incontinence.
What should you do if you suspect you have a UTI?
Not everyone needs to see his or her GP for a simple UTI. Increasing your intake of water at the first sign of symptoms can sometimes be enough to flush out the bacteria before an infection can fully take hold. To help flush out the bacteria causing the urinary infection, it is recommended to drink at least 8 cups of fluid during the day. This may help you feel more comfortable and wash out the bacteria. After a few days, with rest and plenty of fluids, you may not need antibiotics. More severe infections will probably require you to be seen by your GP to consider antibiotics.
Cystitis
There are several preparations available to buy that help to change the acidity of the urine using a chemical called sodium citrate. These can make it more comfortable to pee while you are trying to flush out the infection but are not suitable for people who need to avoid salt. The preparations are often combined with cranberry extracts.
Soda water or bicarbonate of soda
These are similar to the cystitis remedies and aim to make passing water more comfortable.
Paracetamol (follow the directions on the package) or other over the counter medication (discuss with pharmacist) can help by reducing a high temperature and other symptoms. You may find that placing a hot water bottle (wrapped in a small towel) on your abdomen or back soothing.
Sexual intercourse
If possible avoid having sexual intercourse until you are feeling better. You cannot pass the infection onto your partner, but sex can be uncomfortable if you have a UTI.
Post-coital antibiotics help some women by preventing cystitis. These women take a single antibiotic within an hour of having sex to stop the cycle of infection.
When to seek medical advice from your GP or NHS 111
If you are attending a face to face appointment it is helpful if you can provide a sample of urine for the doctor to test.
If your symptoms do not improve within a few days or if:
- you see blood in your urine.
- you are male (over 50).
- you are pregnant.
- your UTI comes back after treatment.
- you notice a relative is confused or agitated.
What medical treatment is available?
Your GP may prescribe antibiotics to treat the urinary infection if there is clear evidence of a UTI. The antibiotics need to be taken as directed. Symptoms should improve within 5 to 7 days.
It is important to finish the prescribed course of antibiotics, even if you start to feel better and your symptoms are improving.
It is advised as best practice to send a urine sample into your GP’s surgery for testing see leaflet ‘Collection of Mid-Stream Sample of Urine (MSSU) for adults’ GHPI1185. Testing a sample of urine is required to find out which, if any, germs (bacteria) are present. If a Urinary Tract Infection (UTI) is identified, appropriate antibiotic treatment can be given. Take the MSSU to your GP’s surgery or laboratory as soon as possible; the sooner it is given in, the more accurate the result will be.
If there are no symptoms of bacteria do not treat unless pregnant.
Treating a recurrent UTI
Sometimes a UTI can come back soon after treatment. Recurrent UTI are described as a repeated UTI with a frequency of at least 3 UTI’s in the last year or 2 UTI’s in the last 6 months. In this situation it is important that a urine sample is sent to the laboratory (microbiology) for testing.
Alternative treatments in preventing a UTI
The risk bacteria becoming resistant to antibiotics is a global problem. In an attempt to avoid the overuse of antibiotics we have identified alternative treatments which are effective in preventing UTIs. ‘Over the counter preparations include:
Cranberry juice or cranberry extract capsules
It is thought that cranberries contain a substance that prevents bacteria sticking to the bladder wall reducing bladder infections. The juices can contain a lot of sugar, which is not suitable for everyone and you would need to drink a lot to be helpful. Instead.
Cranberry capsules are available as an alternative to the juices. There is evidence that they reduce the risk of UTI.
Cranberry supplements should not be taken if there has already been a diagnosis of a UTI, due to the high acid content which can irritate a sensitive bladder.
Cranberry supplements should not be taken if you suffer with diabetes or Irritable Bowel Syndrome (IBS).
If you are taking warfarin please discuss with your doctor as cranberry is contra-indicated with this medication.
The active ingredient of cranberry is D-mannose. D-mannose may be given as a pure ingredient rather than in cranberry products and can be purchased from health food stores.
D-Mannose (200 ml of 1% solution once daily in the evening)
D-Mannose is thought to block E-coli bacteria from growing in the urinary system. It attaches to the E-coli bacteria and prevents it attaching to the cells in the urinary tract. The bacteria are removed on passing urine (voiding).
D-Mannose can cause loose stools and you should check with your specialist doctor or GP before taking D-Mannose. You should also seek advice before taking if you have diabetes as it is a form of sugar.
Methamine Hippurate (Hiprex)
This is a urinary antiseptic which works by destroying different types of bacteria which causes infections. It does require the urine to be acidic for it to be effective. Methamine hippurate is given in tablet form, taken twice daily and can be prescribed by your GP.
This medication works by concentrating in the urine creating a hostile environment which helps to prevent bacteria from growing. Methamine hippurate has an anti-bacterial, anti-fungal or antiviral effect on the bladder and urinary tract.
Methamine hippurate can be used for prolonged periods because it does not develop a resistance like antibiotics.
You must not take this medication if you are severely dehydrated, have a kidney or liver problem, suffer with gout or any metabolic acidosis or chemical imbalance in your blood. This medication should be taken with your GP’s consent.
Topical Vaginal Oestrogen for vaginal dryness:
As hormones change during and after the menopause, the tissues of the vagina can become dry and sore with loss of the ‘healthy’ bacteria and the normal secretions. This dryness is called ‘atrophic vaginitis’ and can contribute to recurrent infections.
Your specialist doctor or GP should be able to diagnose this with a simple examination.
Vaginal creams and pessaries containing oestrogen may help reduce the dryness and the number of infections but can take at least 8 months to work. The decision to use this treatment would be recommended by your GP or a Uro-gynaecologist following other failed preventative measures. A yearly review should be completed by your GP or a uro-gynaecologist.
Further investigations
You may be referred to a specialist urology or uro-gynaecology department if the UTI (s) do not resolve for further investigations.
These investigations may include:
- Ultrasound scan of the bladder and/ or kidney(s)
- Urine flow tests +/- post void bladder scans (portable)
- Cystoscopy to examine inside the bladder.
Contact information
If you have any questions or concerns, please contact:
Gloucestershire Bladder and Bowel Health
Cheltenham General Hospital, Oakley suite 2nd floor Centre Block, Sandford Road, Cheltenham GL53 7AN
Tel 0300 422 5305
Email: ghn-tr.gloscontinenceservice@nhs.net
or
Uro-gynaecology Department
Gynaecology Outpatients, Women’s Centre, Gloucestershire Royal Hospital, Great Western Road, Gloucester GL1 3NN
Tel: 0300 422 624
Further information
Bladder and Bowel UK
Website: www.bbuk.org.uk
Available trust leaflets:
The following leaflets will give you more information please ask the patient’s GP or healthcare professional for copies or visit the Gloucestershire Continence webpage at: www.gloshospitals.nhs.uk/our-services/services-we-offer/continence-service/
- GHPI0531 ‘Bladder urgency and overactive bladder’
- GHPI0533 ‘Fluid and caffeine intake for bladder and bowel health’
- GHPI1412 ‘Improving bowel function and control’
- GHPI1582 ‘Managing bladder and bowel care needs for a person who is suffering with dementia’
- GHPI1185 ‘Collection of Mid-Stream Sample of Urine (MSSU) for adults’