Colposuspension
This page will provide you with basic information about a procedure for stress incontinence known as colposuspension.
On this page
-
What is colposuspension?
-
Do I have to have the operation?
-
What other surgical options are available?
-
Is colposuspension successful?
-
How do I prepare for the surgery?
-
What happens when I come into hospital?
-
What happens after the operation?
-
What should I do about my medication?
-
Risks and complications
-
Problems passing urine after the operation
-
How will the operation affect my sex life?
-
When can I return to my usual routine?
-
Contact information
-
Further information
What is colposuspension?
A colposuspension is a procedure to help women with stress incontinence (leakage of urine when coughing, sneezing or moving). Colposuspension has been used for the treatment of stress incontinence for over 40 years so we have a lot of information about its success and how long it lasts.
The procedure is done either with a bikini line cut in the tummy or through keyhole surgery. Stitches called ‘Burch sutures’ are placed on each side of the bladder neck into the vaginal tissue. The stitches are used to lift up the wall of the vagina and support the bladder and urethra (the tube which you pass urine through).
Not all patients will be suitable to have this operation through a laparoscopic procedure (keyhole surgery). Your surgeon will discuss this with you.
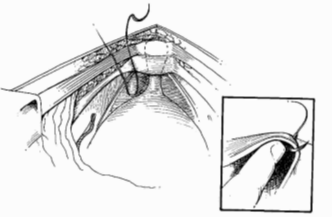
After the procedure, the bladder is supported in a better position, so that the pelvic floor muscles are able to stop urine from leaking once again. The urethra is purposefully slightly kinked by the operation and this makes it harder for urine to leak out.
Do I have to have the operation?
It is difficult to predict how effective the procedure will be as everyone is different. You should only have the operation if you feel that the stress incontinence is badly affecting your quality of life and life style changes and pelvic floor exercises have not been helpful.
The following may ease your symptoms and stop your urinary leakage from becoming worse:
Lifestyle changes
- Reduce the amount of caffeine that you drink for example tea, coffee, fizzy drinks
- Try to lose weight if you are overweight (your GP will be able to advise you)
- Manage a chronic cough if you have one. Stopping smoking will help (please see your GP for smoking cessation advice)
- Try not to get constipated; talk to your GP about ways of helping and treating constipation
- Avoid heavy lifting. You may wish to talk to your employer if your job involves heavy lifting
- Avoid high impact exercise, such as running
Pelvic floor exercises
You may be referred to a physiotherapist who specialises in exercises to improve the control and strength of your pelvic floor muscles.
Medication
Duloxetine can sometimes improve stress incontinence. In some women it works on its own however, it works better when used together with pelvic floor exercises. You can discuss this further with your doctor.
What other surgical options are available?
Other surgical options, apart from colposuspension, are available, such as:
- Para-urethral bulking agent
- Facial sling
Your surgeon will discuss these options with you and provide you with more information.
Is colposuspension successful?
About 80 out of every 100 women feel that their stress incontinence has improved after the colposuspension procedure. However, there are a small group of women for whom the procedure does not seem to work. The procedure is less likely to be a success if you have had previous surgery to your bladder. For most women, the procedure seems to work long term for at least 10 to 15 years. However, some women can experience further problems with their bladder as they get older.
How do I prepare for the surgery?
Before surgery, you will be asked to attend a Pre-admission Clinic to make sure that you are fit and well for your forthcoming surgery. A nurse practitioner or a doctor will ask about your general health, past medical history and any medication that you are taking. You will also be asked about any allergies you may have.
Any necessary investigations such as blood tests, ECG and chest X-rays will be arranged.
You will be given information about the procedure and the care that you will receive. You will also have the opportunity to ask any questions that you may have.
Please make sure that you take a bath or shower before you come to the hospital for surgery. Shaving the perineum is not necessary, however, it is advisable that you trim your pubic hair.
What happens when I come into hospital?
You will be asked to come in for surgery either the day before or the same day as your procedure. You will be seen by the anaesthetist and the surgeon (or a senior member of the team) who will explain what will happen during the procedure. You will be told about the purpose of the surgery and any risks involved. You will be able to ask any questions that you may have before being asked to sign a consent form if you have not already done so.
The operation is usually performed under general anaesthetic (while you are asleep). You will also be given an antibiotic during the operation; this is to reduce the risk of infection.
What happens after the operation?
When you wake up from the anaesthetic you will have a drip (thin tube) going in a vein in your hand. This is to give you fluids. You may have a bandage in the vagina, called a ‘pack’ and a sanitary pad in place. The ‘pack’ is used to apply pressure to the wound to stop it oozing.
A tube (catheter) will be placed in your bladder to drain any urine overnight. The catheter may give you the sensation of needing to pass urine but this is not the case. Usually the drip, pack and catheter are removed in the morning following your procedure.
The day after the surgery, you will be encouraged to get out of bed and take short walks around the ward. This improves your recovery and reduces the risk of blood clots.
It is important that the amount of urine is measured the first couple of times you pass urine after the removal of the catheter. An ultrasound scan of your bladder may be done on the ward to make sure that you are emptying your bladder properly. If you are leaving a significant amount of urine in your bladder, you may have to have the catheter re-inserted into your bladder for a couple of days more.
You will be given anti-embolic (compression) stockings to wear to help reduce the possibility of blood clots. These need to be worn throughout your hospital stay.
You may also be given injections to keep your blood thin and reduce the risk of blood clots. Normally this will be given once a day until you go home but may be longer in some cases.
The wound is not normally very painful but if you need any pain relief, please speak to the nurse looking after you.
You will have some vaginal bleeding after the procedure. This will be like the end of a period and may last for a few weeks.
You will be in hospital for up to 3 to 4 days.
What should I do about my medication?
Let your doctor and pre-operation assessment nurse know about all the medication you take and follow their advice. This includes all blood thinning medications as well as herbal and complimentary remedies.
Risks and complications
The following general complications can happen after any surgery:
- Anaesthetic problems with modern anaesthetics and monitoring equipment, these are very rare.
- Bleeding/haematoma (collection of blood in the wound) - sometimes it is difficult to control bleeding and very rarely you might need a blood transfusion.
- Thrombosis – any period of inactivity will make it more likely that you develop a blood clot in the leg (Deep Venous Thrombosis, DVT). The risk of this happening is reduced by giving you medication to ‘thin’ your blood and by wearing the compression stockings while you are in hospital.
- Wound infection - we will give you antibiotics during the operation. Despite this, some people may still develop an infection. This will usually clear with a full course of antibiotics, but you may need to be in hospital for longer than expected.
- Cystitis sometimes you can get a burning sensation when passing urine, this is caused by a bladder infection. This can happen while you are in hospital or after you have gone home. If the doctor thinks you have a bladder infection you will be advised to take a course of antibiotics. If you experience this once you have left hospital you should contact your GP.
The following complications are particular problems of colposuspension:
- Overactive bladder the bladder becomes irritable or overactive in up to 17 in every 100 of women. This gives symptoms of urgency (needing to rush to the toilet) or frequency (needing to pass urine more often). Sometimes an overactive bladder can make you leak because you cannot get to the toilet in time. You may need medication for this (please ask your GP for advice).
- Prolapse this is a bulge in the vagina caused by the vaginal walls sagging. It is very common and often does not need any treatment. If it happens you may feel a lump or dragging sensation. About 14 in every 100 women who have had a colposuspension procedure are more likely to get a prolapse to the back wall of the vagina. It might be small and may not need treatment. Sometimes if the prolapse is causing symptoms it can be treated with a vaginal pessary (a device inserted into the vagina) or an operation.
- Difficulty passing urine - you might notice that the flow of urine is slower after the procedure. Some women notice that they have to change position on the toilet (such as leaning forward to empty the bladder completely) to get the last of the urine out. About 1 in every 10 women who have had a colposuspension have problems emptying their bladder after the procedure. The next section of this page explains what can be done if this happens.
- Pain during sexual intercourse pain during sex can happen after any operation where there are stitches near the vagina. About 1 in every 20 women find sex uncomfortable or painful after a colposuspension. The sensation during intercourse may be less and occasionally the orgasm may be less intense. This might improve with time.
- Problems with the stitches - in a small number of women, the stitches holding the neck of the bladder in place causes problems. Over time they can wear through to the inside of the bladder. This is rare but may result in bleeding or a persistent discharge (please ask your GP for advice).
Problems passing urine after the operation
Some women have difficulty in emptying their bladder after a colposuspension. This may get better with time, but in a small number of women it lasts forever. It is normal to leave a drop of urine in your bladder after going to the toilet. We call this the ‘residual volume’. However, if too much is left, it can lead to problems such as having to go to the toilet too often and infections of the bladder.
If the residual volume is too high, you may want to learn how to empty your bladder using Clean Intermittent Self Catheterisation (CISC).
This involves emptying the urine that has been left behind using a fine catheter tube.
The catheter is passed along the urethra (water pipe) into the bladder so that the urine can drain into the toilet. Once the urine has been drained, the catheter is removed and thrown away. A new catheter is used each time and they are available on prescription from your GP. Most women use CISC twice a day, but the number of times it is needed will depend on the individual and how her bladder is behaving.
Although passing the catheter into the bladder sounds unpleasant, most women find it is easy to do. Using CSIC gives more control and freedom than using a permanent catheter. The normal feeling of wanting to pass urine is not altered so you will know when to empty your bladder. The catheters are very small and can easily be hidden in a handbag.
How will the operation affect my sex life?
You may resume sexual intercourse when you are feeling comfortable, usually about a month after your surgery. In the long term, there is no evidence to suggest that the operation will make any difference to your sex life.
If you leak urine during intercourse, the operation might make this better, but unfortunately, this is not always the case.
You may benefit from using vaginal lubricant such as KY® jelly, Sylk® or Replens®. These are available to buy over the counter at your chemist.
Some women, during the menopause, may benefit from a course of vaginal oestrogen therapy. This should be discussed with your GP.
When can I return to my usual routine?
You should be able to carry out light activities a few weeks after surgery. We advise you to avoid heavy lifting, heavy household chores, driving and sport for at least 6 to 8 weeks. This is to allow the wounds to heal. Most women need 6 to 8 weeks off work. Please ask your nurse if you need a sick note (also known as a fit note).
Contact information
If you have any problems or concerns after going home, please contact your GP for advice. If your GP is not available contact the:
Urogynaecology Nurse Practitioner
Women’s Centre, Gloucestershire Royal Hospital
Tel: 0300 422 6246
Monday to Friday, 8:00am to 4:00pm
Tel: 0300 422 6278 (answerphone)
Gloucestershire Domestic Abuse Support Service (GDASS)
This is a county-wide service offering a variety of support programmes for women and men over 16 years old who are experiencing domestic abuse.
Tel: 01452 726 570
Monday to Friday, 9:00am to 5:00pm
Domestic Violence Helpline
Tel: 0808 2000 247 (24 hours)
Email: support@gdass.org.uk
Website: www.gdass.org.uk
Further information
National Institute for Health and Clinical Excellence (NICE)
Website: www.nice.org.uk
Website: https://www.nice.org.uk/guidance/ng123
Bladder & Bowel Community
7 The Court, Holywell Business Park, Northfield Road, Southam CV47 0FS
Tel: 01926 357 220
Email: help@bladderandbowel.org
Website: www.bladderandbowel.org
British Society of Urogynaecology
27 Sussex Place, Regent’s Park, London NW1 4RG
Email: bsug@rcog.org.uk
Website: https://bsug.org.uk/pages/information-for-patients/111
International Urogynecological Association (IUGA) Your Pelvic Floor
Website: https://www.yourpelvicfloor.org
We hope that you have found this page helpful. If you have any further questions, please feel free to ask your surgeon.